

A Cancer Vaccine Is Born
Last fall’s announcement of a vaccine against cervical cancer came as
a stunning breakthrough in medical science, but it was only the latest chapter
in a pioneering, Rochester-born effort begun two decades ago. By Corydon Ireland
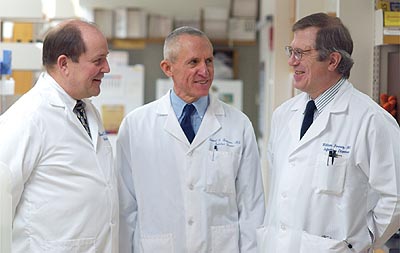 |
| SCIENCE TIMES: Rose, Reichman, and Bonnez worked for more than two decades on the technology behind a new cervical cancer vaccine. |
Room 3-5135 at the Medical Center looks like a hundred other cubbyholes of basic science. A gray metal door decorated with the obligatory cartoon leads into a space the size of a motel room. White lab coats drape on wire hangers. Plain shelves, a desk, and a computer surround a breast-high bench arrayed with instrumentation. The paint scheme: early dorm room.
“The posters are to cover the holes in the walls,” jokes William Bonnez, an associate professor of medicine and a veteran researcher who says not much has changed inside the room in a quarter century.
But this is no ordinary workspace, and some day it may merit a plaque. Here, starting more than two decades ago, Bonnez and University colleagues Richard Reichman, a professor of medicine, and Robert Rose ’94M (PhD), an associate professor of medicine, developed the key technology behind two vaccines that may eliminate cervical cancer, a disease that each year kills 250,000 women internationally, including 4,500 Americans.
One vaccine using the Rochester technology is Gardasil, developed by pharmaceutical giant Merck, that’s expected to be on the market some time this year.
Another candidate is Cervarix, developed by GlaxoSmithKline, that could be ready by 2008.
Gardasil “is a phenomenal breakthrough,” Gloria A. Bachmann told Newsday last fall when results of the final trial for the vaccine were released. She’s director of the Women’s Health Institute at the Robert Wood Johnson Medical School in New Jersey and was not involved with the Rochester research. Such a vaccine, Bachmann adds, “promises to take this entire chapter (of cervical cancer) out of women’s lives.”
Last fall, Merck announced that in a final large trial Gardasil was nearly 100 percent effective in prompting immunity against the most troublesome forms of the human papillomavirus (HPV), a family of sexually transmitted viruses associated with diseases of the reproductive system and skin. Two of the types (HPV16 and HPV18) cause 70 percent of the cervical cancers diagnosed worldwide.
The study of more than 12,000 sexually active women ages 16 to 26 worldwide,
the company reported, showed that after two years, those who had received the
vaccine remained free of the four troublesome strains of HPV. Based on its results,
Merck has applied for FDA approval to begin selling Gardasil this year.
While the vaccine is not the first to thwart a known cancer—the vaccine
for hepatitis B seems to prevent some forms of liver cancer—it is the
first designed to protect humans against an identified cancer-causing agent.
The announcement prompted headlines around the world, but largely unreported was the remarkable story of the Rochester virologists whose innovation, dedication, and perseverance resulted in the key breakthrough that lies at the heart of the vaccine.
Reichman, a native of Utah who still has the skiing habit he acquired in the West, moved to Rochester in 1982 from the University of Vermont. A mentor in New England had told him that HPV and genital tract cancers included uncharted territory, and were worth exploring as a life’s work.
 |
“The pure biology of viruses is fascinating.”—Bonnez |
Bonnez, whose father and grandfather were both Resistance fighters in France during the Nazi occupation, grew up in the 1950s working-class suburbs of Paris and took his medical degree at a military college. He gave up an early dream to be a colonial physician in Africa to move to the United States to study viruses, the smallest infectious agents known.
“The pure biology of viruses is fascinating,” says Bonnez, whose adolescent reading was seasoned with tales of Louis Pasteur and other medical adventurers interested in saving lives by studying infectious agents. What also drew him into virology was the idea that advances in the basic science of viruses could segue into the practical realm and have real meaning in clinical settings.
Rose took an intriguingly crooked path to the study of viruses. His first job
was as a railroad brakeman, the start of a steady climb up the ladder at the
Erie Lackawanna Railroad. But frustration derailed his first career.
“One day I said: ‘I don’t like this,’” Rose recounts.
“‘I’m going to go to college.’” He enrolled as
a freshman at the State University College of New York at Geneseo, and emerged
in 1984 as a magna cum laude biology and chemistry graduate. That year, he started
as a laboratory technician at Rochester and before long took his seat at the
bench in Room 3-5135.
The three didn’t set out to find a cancer vaccine. Instead, they were looking for a simple blood test that would allow doctors to see whether a woman was infected with a strain of HPV and whether that strain was linked to cancer.
Almost immediately, they hit a major roadblock. Such tests hinge on finding an “antigen,” the foreign protein in an invading virus that triggers an immune response. Faced with the antigen of an invading microorganism, the bloodstream floods with antibodies, the custom-made proteins that kill or neutralize the invaders.
To find the right antigen, the team needed plenty of virus to work with. But HPV doesn’t grow in standard tissue cultures, and it’s hard to extract in useful amounts from genital warts and other tissue. Says Bonnez: “We had to find a substitute.”
Like other researchers at the time, the team turned to papillomaviruses from cows. The French researcher set out to find bovine warts, in quantity—surely one of science’s oddest shopping trips. Bonnez phoned veterinarians for help and visited slaughterhouses and dairy farms (“I ruined one pair of pants,” he says). Once in the lab, the cow warts were painstakingly minced and purified with a mix of enzymes.
To find out if the purified virus from cow warts would work as an antigen, it had to be tested on human blood, which was easy enough to get. Three out of every four sexually active humans—5.5 million adult Americans—every year get an HPV infection from a partner sometime in their lives.
But a control was needed—blood from humans who professed never to have had any sexual contact, the chief route of infection from HPV viruses. Uninfected adults were hard to find.
So an unusual cohort of people came to the rescue—a group of Rochester-area nuns and priests. Bonnez polled the volunteers on their sex lives and asked them to give blood samples. “I did it myself—I was not embarrassed,” he says of his unorthodox hunt. “It was really the key to finding a (blood test) that worked.”
By 1986, the University researchers were becoming convinced that the antigen they developed from the bovine papillomavirus was not the right one, since it had no relationship to human disease. “It was a lot of work,” sums up Reichman, “for not very much.” To complicate matters, says Bonnez, the scientific literature of that time was full of “false leads” still pointing to cows as the key to an antigen for HPV. “It slowed things up,” he says.
The team turned to E. coli, a type of bacteria that looked promising as a source for the kinds of proteins that would be crucial to detecting antibodies in infected blood. But to be useful, proteins have to fold in just the right way, and the E. coli proteins proved problematic.
The team turned in another direction: moths and “nude” mice.
Manipulating the cellular system of moths, the team was able to make proteins that would masquerade as infectious viruses. Relying on baculovirus, a cigar-shaped insect virus roughly 300 nanometers long, the team used the moth system to make recombinant proteins that tended to fold properly.
Rose made the baculovirus the subject of his 1990 master’s thesis. To this day, he has an electron microscope image of one on his office wall, right next to photos of his wife and children.
The hairless nude mice (called “nude” because the animals have “naked” immune systems that, by design, are severely compromised) were used to grow HPV11, a virus that causes genital warts in humans.
By 1990, it was breakthrough time. Using a purified form of the viral particles, the researchers immunized rabbits, two of which developed antibodies to HPV11. It was the first hint that the work might go beyond a blood test and be the basis for a lifesaving vaccine.
After six years of tedium, false starts, hard work, and a dearth of written research, says Bonnez, “for the first time, I saw we had something good.”
An antibody response in the rabbits meant that it was possible to block infection from a single type of the HPV virus. “This was perfect,” says Rose. “This was beautiful, because it meant that a vaccine was possible.”
But a scientific challenge remained. A working human vaccine would require a noninfectious form of the HPV virus—one that would replicate the shape of the harmful virus without replicating its danger to humans. The researchers needed to make lots of these shapes, called noninfectious capsids. Resembling a soccer ball, the shape of the virus is built from 360 copies of the protein that forms HPV’s outer coat. (The icosahedral shape is the favored form of many viruses.)
At this point, salvation took another turn. In 1990, Rose attended a virology conference in Salt Lake City, Utah, where some HIV researchers talked about “virus-like particles,” or VLPs. The noninfectious particles “self-assemble” within infected cells and can elicit immune responses—in the form of antibodies—without causing disease.
At Rochester, Rose inserted the gene for the HPV coat, or capsid, into the baculovirus. The sought-after noninfectious particles, which took on the shape of their infectious cousins, were formed. The particles provoked the same immune response as an infectious virus but caused no disease.
Making the “empty capsids” was the subject of Rose’s 1994 Ph.D. dissertation. By the time he got the degree, he had helped write three papers on the breakthrough and had applied for a patent.
Rose’s dissertation work didn’t just sit on a shelf, noted David Guzick, dean of the School of Medicine and Dentistry in a 2005 “Dean’s Newsletter.” Rose is more modest, calling his accomplishment “a reduction to practice.” That’s when research, to use a popular phrase among scientists, goes from “bench to bedside”—from the realm of the theoretical into the realm of the practical.
But the vaccine’s journey from bench to bedside included some legal pitfalls. The technology was licensed in 1993 to Praxis, then a small pharmaceutical company in Rochester. But the company was bought out by American Home Products, which declined to pursue the vaccine work. In 1994, the patent was returned to the University.
“Then we were really high and dry,” says Reichman. “We had no one to help us.”
Getting a patent returned “is always a hard situation for universities,” with its implication that the technology is not worthy, says Robert Goodwin, president of LygoCyte Pharmaceuticals in Montana. During the 1990s, while a technology transfer specialist at Rochester, he helped secure critical funding for developing the vaccine. “A vaccine against cervical cancer,” he says, “was an untested market.”
Especially needed is an outside partner. Even in the best of situations, says Goodwin, universities are not prepared to go beyond research to manufacture and test something like a vaccine.
Reichman credits Goodwin (“He was a dream”) with rescuing the idea of an HPV vaccine. He came across MedImmune, a small company in Maryland that would take on the project and assume the patent rights. The company made a test vaccine in sufficient amounts for Rochester to conduct the first human trial, a near-perfect Phase 1 that looked at 64 people. It proved that the harmless virus-like particles were safe and could induce antibodies that block an HPV infection.
MedImmune then sublicensed the technology to GlaxoSmithKline, a transfer that delayed further testing on humans.
Michael Goldman, a patent attorney with the Rochester law firm of Nixon Peabody, helped shop for a partner in the pharmaceutical world for Rochester’s vaccine work, including Merck’s eventual interest. “Without him, we’d be lost,” says Reichman.
A chemical engineer by training and a one-time U.S. Patent Office worker, Goldman had earlier been hired to help fight the legal “interference” battle with other institutions working on the VLP concept.
“Part of the challenge was getting the companies to believe we were a horse worth putting money on,” Goldman says. “It was a race.”
That race involves three other institutions: the National Institutes of Health, Georgetown University, and the University of Queensland in Australia. And it’s worth running, says Goldman.
An HPV vaccine could represent a new global market worth $2 billion a year. “This is high-stakes patenting and litigation,” he says.
In 2005, Merck and GSK signed a revenue-sharing agreement on future HPV vaccines. Royalties will get distributed to the University and its institutional rivals.
Georgetown eventually won the U.S. patent fight over the HPV/VLP technology because its technical papers were published first. But last May the Rochester team won a European patent for the HPV16 vaccine and has since won a parallel patent in Australia.
In the patent fights, says Goldman, the University’s key argument comes down to a single word: “workable.” The Rochester technology, in contrast to the three competitors’, involves a vaccine that’s based on solid preclinical evidence and that has proven itself in a human trial.
Rochester’s share is difficult to estimate without disclosing the confidential royalty rate in the 2005 agreement, says Marjorie Hunter, a former federal and corporate patent attorney and now director of the Medical Center’s Office of Technology Transfer. But royalties will likely be “several millions” of dollars a year over 10 years, she says, which would put the HPV vaccine in the University’s top three for earnings.
“It’s not all about the money,” says Hunter, who for six years was technology transfer director for the federal Centers for Disease Control and Prevention. “Things like the HPV technology point out the real purpose—seeing results at the patient’s bedside, seeing lives saved.”
Saving lives is “the net good” for technology transfer, says Hunter. “That’s how it fits best into a University’s mission.”
For their part, the researchers are modest about their achievement. But occasionally they reflect on affecting the health of so many.
“It’s been an amazing life experience,” says Rose. “It’s been thrilling—that what we’ve done could affect the world.”
Corydon Ireland is a Rochester-based freelance writer.
