Features
 PAPER TRAIL: Arthur Moss ’62M (Res), a professor of medicine, and his clinical research teams have collected data from thousands of cardiology patients in a quest to develop improved therapies for heart disease. (Photo: Adam Fenster)
PAPER TRAIL: Arthur Moss ’62M (Res), a professor of medicine, and his clinical research teams have collected data from thousands of cardiology patients in a quest to develop improved therapies for heart disease. (Photo: Adam Fenster)When Arthur Moss ’62M (Res), a professor of medicine at Rochester, arrived at Massachusetts General Hospital as an intern in the late 1950s, he found a teacher and mentor who gave him a model for his own life as a cardiologist. Paul Dudley White, the chief of cardiology at Massachusetts General and cardiologist to former president Dwight Eisenhower, founded the American Heart Association. He established Massachusetts General’s cardiac unit and through his clinical research, he improved the care of patients with heart disease.
Today, Moss credits White—who was Moss’s teaching attending physician through his six-week internship—with showing him how a physician could both care for individual patients and discover new ways of treating disease.
“I wanted to see patients in a clinical setting, and advance the science of cardiology,” Moss says of his aspirations for a career that, five decades on, has contributed to saving the lives of countless people.
Moss has done that by collaborating with other cardiologists, geneticists, epidemiologists, biostatisticians, and a host of others; he has involved thousands of patients who have volunteered to take part in his teams’ research—all in a quest to better understand heart disease and to develop more effective therapies for cardiac patients.
The world’s foremost expert on long QT syndrome—a condition that puts patients at risk for sudden cardiac arrest—Moss was one of the researchers who discovered the genes responsible for the disorder. For more than 20 years, he has led a team of cardiologists in reducing potentially fatal cardiac arrhythmias through advances in drug treatment, such as beta blockers, and through devices like implantable cardioverter defibrillators.
One concern unifies his years of research.
“All of our studies have related, in one way or another, to the question, ‘How can we improve treatment for patients with heart disease?’ ” Moss says.
The importance of harnessing science for practical solutions to health problems may seem obvious, but in recent decades some policymakers have argued that the nation’s biomedical focus has drifted away from research that’s directly applicable to patients and human disease. Congress and the National Institutes of Health (NIH) are seeking to change that, and Rochester is helping to lead the way.
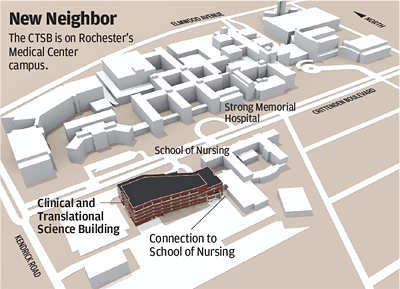
This spring, Rochester will dedicate the new Clinical and Translational Science Building (see page 28). Built with the help of a $50 million grant from the state of New York, it’s one of the first facilities in the country constructed specifically to serve as the academic home for clinical and translational science at an academic health center.
It’s also the physical manifestation of a renewed emphasis on clinical research at Rochester. In 2006, the School of Medicine and Dentistry was one of 12 top academic health centers to receive a Clinical and Translational Science Award from the NIH. The $40 million dollar grant, the largest NIH award in Rochester’s history, is helping the University and its partner institutions to bring together the people, technologies, and infrastructure needed to speed the pace at which advances in biomedical research make tangible improvements in people’s lives.
Together, institutions receiving the awards—there are currently about 55—form a national consortium on clinical and translational science. “The development of this consortium represents the first systematic change in our approach to clinical research in 50 years,” Elias Zerhouni, then director of the NIH, said when announcing the first awards in 2006. “Working together, these sites will serve as discovery engines that will improve medical care by applying new scientific advances to real world practice. We expect to see new approaches reach underserved populations, local community organizations, and health care providers to ensure that medical advances are reaching people who need them.”
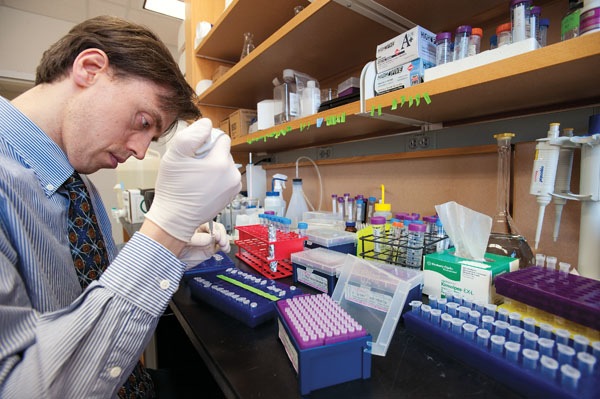 INCREMENTAL PROGRESS: Thurman Wheeler, an assistant professor of neurology, works with colleagues at the lab bench and in
clinical research on patients to find a treatment for muscular dystrophy. (Photo: Adam Fenster)
INCREMENTAL PROGRESS: Thurman Wheeler, an assistant professor of neurology, works with colleagues at the lab bench and in
clinical research on patients to find a treatment for muscular dystrophy. (Photo: Adam Fenster)Since World War II, the United States has given priority to funding basic science, and breakthroughs in molecular and structural biology, neuroscience, genetics, and bioengineering are rich with potential to transform the diagnosis and treatment of diseases. But that potential has been slow to be realized, in part because of the disconnect between basic science—which is concerned with components of organisms, such as cells and genes—and clinical science, which applies those findings to people.
The NIH award aims to reduce the time required for lab discoveries to produce patient treatments, to engage communities in the work of clinical research, and to train new generations of clinical and translational researchers.
“This isn’t about basic versus clinical research,” says Thomas Pearson, the senior associate dean for clinical research at the School of Medicine and Dentistry and principal investigator of the NIH grant. “The point is, the basic science program is a great pitcher; it’d be awfully nice to have an equally great catcher. You need both sides to play baseball.”
According to Bradford Berk ’81M (MD/PhD), CEO of the Medical Center and senior vice president for health sciences, Rochester has a strong tradition of both basic and clinical science. “This medical school is steeped in the legacy of founding dean George Whipple, himself an iconic translational scientist,” Berk says. “Our new Clinical and Translational Science Building is an integral element of the Medical Center’s strategic plan. It will serve as a conduit for rapidly bringing basic science discoveries to everyday patient care.” The new building—a four-story, 200,000-square-foot structure—provides an integrated academic home for clinical research at Rochester. It will bring together all of the disciplines needed to transform creative scientific insights into proven, effective therapies.
Now there will be a critical mass of clinical researchers under one roof: several hundred people who are involved in the enterprise of translational research, from biostatisticians and bioethicists to clinical trial researchers and researchers in specific areas such as cancer, neurology, cardiology, smoking cessation, and obesity prevention and management. The building has an open floor plan to encourage interaction, and also provides substantial space for community involvement. Participation by research volunteers is a key piece of clinical research.
“The building’s a structural icon, but what’s magic is that it’s allowed us to restructure and reorganize from the inside out: research-friendly and research-participant friendly,” says Karen Mustian, an assistant professor of radiation oncology who also holds an appointment in the Department of Community and Preventive Medicine. Joining the Medical Center in 2003, she set up a lab to support her own research on the therapeutic benefits of exercise for cancer survivors and those undergoing cancer treatments.
With support from the institute, Mustian’s lab has evolved into the Physical Exercise and Activity Kinesiology Clinical Research Core Lab, a resource for other clinical researchers concerned with tracing connections between physical activity and disease mitigation or prevention.
“The inception of this lab as a core facility and the support we’ve received from the University really exemplifies the fact that this is what the University wants to see increased focus on—providing infrastructure for outstanding clinical science,” Mustian says.
The plan for a dedicated building designed specifically to support clinical research strengthened Rochester’s application for an award, says Pearson, coauthor of the application.
Rochester’s established history also helped. In addition to Whipple, the medical school’s founding dean who earned a Nobel Prize in 1934 for his research leading to the use of raw liver as a treatment for pernicious anemia, more recent researchers have contributed such pioneering advances as the use of lung surfactant to help premature infants survive and the development of the HiB vaccine, which has nearly wiped out childhood meningitis. Rochester scientists also contributed to the discovery of a method to prevent many instances of cervical cancer, the HPV vaccine.
Extending the Medical Center’s Clinical Research
The Upstate New York Translational Research Network, part of the Clinical and Translational Science Institute, aims to increase the quality and quantity of translational research in the region. Participating institutions include:
- University at Buffalo, State University of New York (SUNY)
- Upstate Medical University in Syracuse
- Trudeau Institute
- Masonic Medical Research Laboratory
- Rochester Institute of Technology Wadsworth Center, New York State Department of Health
- Roswell Park Cancer Institute
- Rensselaer Polytechnic Institute
- SUNY Binghamton
- Cornell University
- Ordway Research Institute
- Albany Medical College
- Albany School of Pharmacy
- Bassett Healthcare System in Cooperstown, N.Y.
- Guthrie Healthcare System in Sayre, Pa.
A wide-reaching biomedical research consortium—the Upstate New York Translational Research Network—expands the Medical Center’s clinical research to encompass a region of about 6 million people. The demographically diverse area includes several understudied groups, such as rural communities, a substantial Native American population, and Rochester’s large deaf and hard of hearing community.
Mark Taubman, dean of the School of Medicine and Dentistry, says enhancing clinical and translational science is fundamental to delivering on the Medical Center’s promise.
“As an academic medical center, our number one goal is to make discoveries that will improve the health of our population—our region first, but also the world.”
One way that making a priority of translational science will benefit people’s health is by creating the infrastructure necessary to help turn discoveries made in the lab into clinical applications.
“Basic discoveries that can improve health often hit a roadblock in being translated to clinical use. That roadblock is expense, and academic medical centers didn’t have the infrastructure to do that,” Taubman says. “The NIH saw we’d have to develop infrastructure to help academic medical centers get discoveries to users, to take them ‘from bench to bedside.’ ”
Research on muscular dystrophy conducted by a team of physician-scientists led by Charles Thornton, a professor of neurology, illustrates the complexity of the process.
“I came to Rochester in 1989 to join a project on finding a treatment for muscular dystrophy. And I’ve never stopped working on this,” Thornton says. He and a team of fellow neurologists have been working to understand how a genetic flaw leads to myotonic dystrophy, the most common form of muscular dystrophy in adults—and they’ve found a way to treat it in mice. Their work has been necessarily incremental—but it has also advanced on multiple fronts, says Thornton, who both sees patients and works in the lab.
Thornton and his colleagues—Richard Moxley, the Helen Aresty Fine and Irving Fine Professor of Neurology, and Chad Heatwole and Thurman Wheeler, both assistant professors of neurology—have taken a two-pronged approach to their research. One prong has been patient-oriented, with clinical research to answer questions such as how the disease progresses in people, and how the disease’s progress and response to treatment can best be measured.
“The other prong is on the bench research side,” Thornton says, “to understand how an abnormal gene causes the symptoms of disease, to create animal models that recapitulate the disease process, and to devise targeted treatments to try to reverse symptoms. That’s the stage we’re up to now. We have things we think are working well in animal studies.
“What we’ve done simply is to follow the classical paradigm that people were hoping would work, in the sense that we’d take our new understanding of molecular genetics and use it to devise very targeted treatments of diseases that were incurable.”
It’s a “vertically integrated” approach, says Thornton, with basic science discoveries about the disease, developments of potential treatments, and clinical research on people with myotonic dystrophy all happening simultaneously.
“We’ve devoted years of effort, and so have hundreds of patients, to the enterprise of knowing in advance—when something’s ready to test—how to test it really efficiently,” he says.
That level of preparedness is key because the stages involved in bringing a treatment to fruition add up to many years of work.
Thornton and his team so far have results they are heartened by. They’ve achieved good effects in genetically engineered mice, involving the reversal of features of the disease. “If we can translate that into people it has a possibility of transforming the lives of people with the disease.”
Knowledge of the impact that their work can have drives team members to work nimbly and prudently, committed not to particular methods or schools of thought but only to a final result.
The research “started with, and has always been driven by, the desire to find a treatment that can really improve the lives of our patients using the fastest, cheapest, most effective path we could find,” Thornton says, “with no attachment to one theory ever allowed, always trying to keep ourselves attached to whatever could get us where we wanted to go in the shortest period of time.”
Such practicality is central to clinical and translational research, says Taubman, and it’s another way in which the enterprise can benefit health care.
“There are a lot of things out there on the prevention, diagnostic, and treatments sides that we don’t know how good they are,” he says. “There’s a whole area of research—it’s called comparative effectiveness research—that’s trying to understand, Are current treatments and diagnostic tools the best? What increases quality and decreases cost?”
 COMMUNITY TIES: Nana Bennett, the director of the Center for Community Health and a professor of medicine, says health care
providers and communities must work together in solving health problems. (Photo: Adam Fenster)
COMMUNITY TIES: Nana Bennett, the director of the Center for Community Health and a professor of medicine, says health care
providers and communities must work together in solving health problems. (Photo: Adam Fenster)They’re questions that occupy Nana Bennett, a professor of medicine and director of the Center for Community Health. Focused on prevention, the center aims to make Rochester a healthier place.
“We’re really focused on what I call the end stage of translation,” says Bennett.
“Academic research centers have an obligation to be responsive to public health needs of their communities, and that hasn’t been traditionally the case. We need to nurture that.”
The World Health Organization ranks life expectancy in the United States—70 years—at 24th in the world. Less than 2 percent of the country’s health care spending goes toward prevention, and scientific advances are slow to make their way into people’s daily lives—not just new drugs, but ways chronic disease can be managed, and new insights into how people can take control of their own health.
Clinical trials can determine whether a given device or drug or behavior is effective, Bennett says, but there are more questions to be answered. How can new information best be disseminated to the medical community? How well do measures work when they move beyond the comparatively small groups participating in a clinical trial and into the general population? What are the most effective ways to educate the public?
If discoveries produced by basic science are going to improve the nation’s health, she says, researchers have to work with the community. The Healthy Living Research Center that Bennett oversees is an effort to do just that. She calls it a “unique marriage of clinical behavior change services and behavior research.”
Bennett cites a 2007 study in the New England Journal of Medicine showing that 40 percent of instances of premature death in the United States can be attributed to behavior; social circumstances are at the root of another 15 percent.
“If you want to improve health, you need to go after these things.”
The Center for Community Health—which has run focus groups to learn more about demographic groups’ feelings about clinical research and participating in it—works with community organizations, individual community members, and medical practices to improve community health and to gather data that feeds further research.
“It’s the ultimate test of something’s implementability” to see what happens when it reaches patients in their doctors’ offices, says Pearson.
The path from the bench to the bedside and back again is one shaped by rousing ambitions and gritty practicalities. They’re inextricable, Moss suggests.
“What we’ve tried to transmit to our cardiology fellows is that with their specialized knowledge, they have a responsibility for applying that knowledge to patients—but also a responsibility to advance the fund of knowledge.”