Features
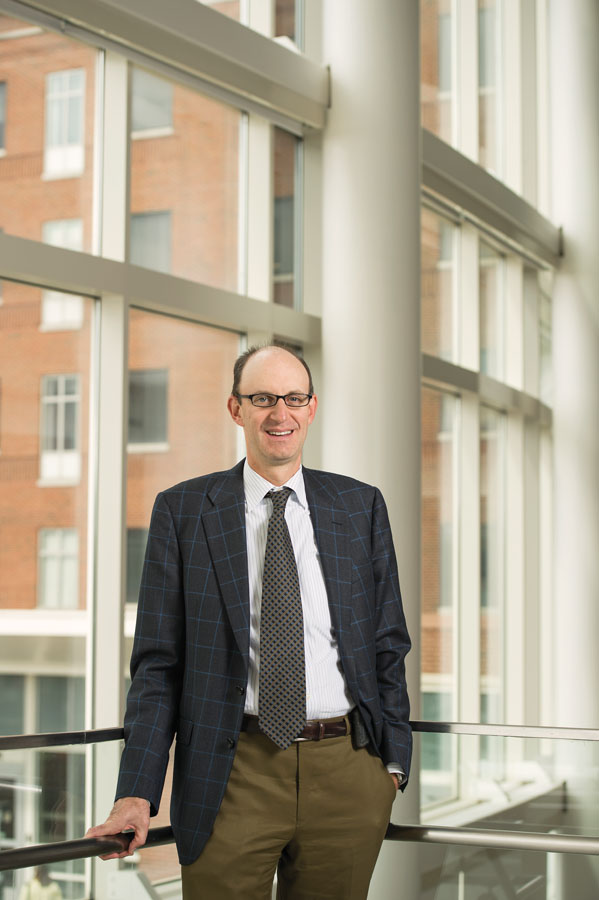 PATIENT FOCUSED: Physicians, researchers, and caregivers use their experience with patients to help guide their plans for
the Wilmot Cancer Institute, says director Jonathan Friedberg. (Photo: Adam Fenster)
PATIENT FOCUSED: Physicians, researchers, and caregivers use their experience with patients to help guide their plans for
the Wilmot Cancer Institute, says director Jonathan Friedberg. (Photo: Adam Fenster)Four decades after President Richard Nixon signed the National Cancer Act of 1971, launching what was to be a full-scale attack on the deadly disease, the battle wages on.
The disease is responsible for one out of every four deaths in the United States. That’s approximately 1,600 people every day. The American Cancer Society estimated that there would be 1.6 million new cancer diagnoses in 2014 alone. Medical expenditures connected to cancer cases are expected to reach between $158 and $207 billion by 2020, according to the National Cancer Institute (NCI).
But there’s been a great deal of progress. Because of early detection, more sophisticated treatment, and greater awareness of the disease and its symptoms, nearly 14.5 million adults and children in the United States can call themselves cancer survivors.
Rochester has been an important part of that story from the beginning. Tracing its roots to the Department of Medicine at Strong Memorial Hospital in the 1970s, the University’s first cancer center grew out of the Division of Oncology. In 1974, a team led by Robert Cooper, a surgical pathologist, applied for an NCI grant to support a specialized center that would encompass clinical care, have the ability to conduct clinical trials, and have the capacity to do important basic research.
 PRECISION CARE: By identifying a gene abnormality in the lung cancer of Sharon Billington (right) of Adams Basin, New York,
Wilmot physicians matched her treatment to a therapy targeting the gene. Billington received weekly treatments from caregivers
like registered nurse Corinne Porter. (Photo: Adam Fenster)
PRECISION CARE: By identifying a gene abnormality in the lung cancer of Sharon Billington (right) of Adams Basin, New York,
Wilmot physicians matched her treatment to a therapy targeting the gene. Billington received weekly treatments from caregivers
like registered nurse Corinne Porter. (Photo: Adam Fenster)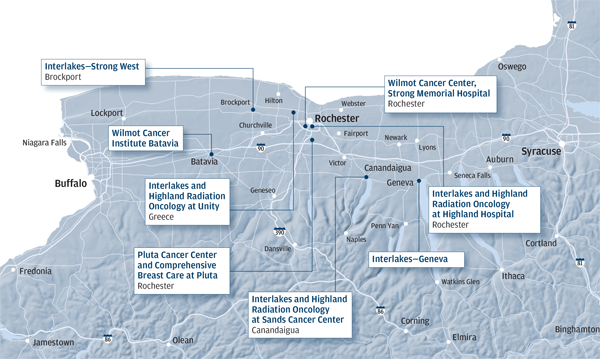 (Illustration: Steve Boerner)
(Illustration: Steve Boerner)The Launch of an Institute
As part of the recognition of the University’s 40 years of leadership in the research, diagnosis, and treatment of cancer, the main institutional home for that battle was renamed the Wilmot Cancer Institute last summer.
The new name reflects a revamped organizational structure for all of the University’s clinical and research programs in cancer, including a growing presence throughout western and upstate New York.
With the James P. Wilmot Cancer Center as its hub, the institute encompasses a network of treatment facilities and all cancer research activities at the University. As part of an effort to expand and deepen the institute’s mission, UR Medicine also launched a $30 million comprehensive campaign with a focus on cancer research.
The institute is designed to provide the highest level of care by making the expertise and capabilities of clinicians, faculty, and health care professionals available to patients without traveling far from home.
 FAMILY SUPPORT: Judy Wilmot Linehan (left), the late William Wilmot, and Thomas Wilmot Sr., a University trustee, helped kick
off a $30 million campaign for the Wilmot Cancer Institute. (Photo: Adam Fenster)
FAMILY SUPPORT: Judy Wilmot Linehan (left), the late William Wilmot, and Thomas Wilmot Sr., a University trustee, helped kick
off a $30 million campaign for the Wilmot Cancer Institute. (Photo: Adam Fenster)A Family Tradition
Judy Wilmot Linehan has seen the toll that cancer can take on a family, but she’s also seen progress against the disease over the past decades, particularly by researchers and clinicians at the Medical Center.
Linehan is part of three generations of the Wilmot family who have provided leadership support to the cancer center that bears the name of her father, a former University trustee. This spring, she added to that legacy when she and her brothers, Tom and Bill, announced a $4 million gift from the family and from the James P. Wilmot Foundation to support research initiatives and to establish the Wilmot Distinguished Professorship in Cancer Genomics. Bill Wilmot died in fall 2014, not long after the announcement.
“It has been amazing watching the progress in cancer research and patient care at Wilmot since 1980,” Linehan said at the launch of a $30 million campaign to support the Wilmot Cancer Institute. “We are thrilled to participate in its continued progress. Our family has been so affected by this terrible disease. It has taken away some of the most important people in my life. It is truly our pleasure to support the Wilmot Cancer Institute. I can’t wait to see what it will accomplish.”
The Wilmot family’s philanthropic commitment to cancer research began in 1981 when the Wilmot Foundation funded the Wilmot Fellowship Program. The effort provides funding to train physicians, including such scientists as William Bonnez of the University’s HPV vaccine team, to pursue careers in cancer research around the world.
Since the program was established, the Wilmot Foundation and the Wilmot family have donated tens of millions of dollars to the University to support cancer research and treatment. Carrying on the Wilmots’ tradition, members of a third generation of the family serve in leadership positions on the institute’s board.
In 1975, the University became one of the first to receive such a core grant. Over the past 40 years, the University’s multipronged effort to understand the biology of cancer, as well as to offer state-of-the-art treatment and care, has grown into a nationally recognized program.
In 2014, those initiatives were brought together under the umbrella of the newly established Wilmot Cancer Institute, a multisite hub for research and treatment.
The institute oversees eight satellite treatment facilities, as well as cancer research and treatment activities at the Medical Center. The institute cares for about 10,000 people each year.
“The University of Rochester has made monumental strides in the past 20 years in improving their global and diverse attack on cancer and the biology of cancer,” says John DiPersio, chief of oncology at Washington University School of Medicine in St. Louis, where he also serves as deputy director of the Siteman Cancer Center.
“They are one of the unique centers in the country now that has an actual destination for their cancer patients; most others are integrated into the hospital setting.
“They’ve also allocated enough resources into that same site to have a critical mass of researchers and patients for both basic and translational care.”
Working on Vaccines
“Without question, one of the contributions that has had the most impact has been the cervical cancer vaccine,” says Jonathan Friedberg, director of the Wilmot Cancer Institute, the Samuel E. Durand Professor, and chief of hematology and oncology. “It has the capacity to prevent cancer in hundreds of thousands of people, and has become standard routine practice in the United States.”
In the 1990s, William Bonnez ’89M (Flw), associate professor of medicine, Richard Reichman, professor of medicine, and Robert Rose ’94M (PhD), associate professor of medicine, developed a technology to target human papillomavirus (HPV)—the virus that causes cervical cancer.
The technology was instrumental in two vaccines—Gardasil and Cervarix. Before the vaccines, cervical cancer was estimated to kill 250,000 women each year, including 4,500 in the United States. The vaccines, the first designed to offer protection against an identified cancer-causing agent, are recommended for both girls and boys by the World Health Organization, the Centers for Disease Control and Prevention, and the American Academy of Pediatrics.
Developing More Precise Treatments
Based in the idea that by analyzing the underlying genetic and biological underpinnings of each patient’s disease, precision medicine is a leading focus of research at Wilmot and other centers in the United States.
Examples include testing for patients with chronic lymphocytic leukemia to identify mutations to a particular gene that prevent standard chemotherapy from working and building molecular profiles of lung cancer tumors to see if patients can be better matched with targeted therapies through clinical trials.
And in treating breast cancer, accurate measurement of specific genes has become an important factor in new treatments for many patients
Such targeted strategies are also seen as key to treating pancreatic cancer, which can be one of the most deadly forms of the disease and resistant to many standard treatments.
This fall, noted cancer surgeon and pancreatic cancer specialist David Linehan joined the Medical Center as the Seymour I. Schwartz Professor and chair of the Department of Surgery.
With experience as a clinician, surgeon, and researcher, Linehan also serves as the institute’s director of clinical operations. Linehan specializes in treating cancers of the liver, pancreas, and gastric and biliary tract, and has earned recognition for bringing novel and innovative therapies to patients with hard-to-treat cancers.
He joins Wilmot investigators—including Wilmot’s director of research, Hartmut (Hucky) Land—already in the midst of a five-year, $2 million study investigating a gene network that controls the progression of pancreatic cancer.
Assessing the Needs of Seniors
Despite the fact that 70 percent of cancer survivors are over age 65, there is a widely acknowledged lack of safe and effective treatment approaches for older adults, whose health concerns are often accompanied by particular physical, psychological, and social issues. Wilmot’s Geriatric Oncology Clinic is one of fewer than 10 similar clinics nationwide offering multidisciplinary resources, grant support, and models of care designed around careful study of collected data.
To have such features located in a medium-sized institution is unusual, “and our program is one of the largest,” says clinic director Supriya Mohile, an associate professor of hematology and oncology who has earned a national reputation for her work with older cancer patients. “We’re one of maybe three that has two geriatric oncologists. Most centers only have one.”
The field of geriatric oncology is relatively new, formalized in 2000 with the creation of the International Society of Geriatric Oncology, and will be increasingly relevant given predictions that 20 percent of patients over age 65 will be diagnosed with cancer by 2030.
Despite that statistic, no consistent protocol exists among oncologists or geriatricians about the best ways to care for older people with cancer. At the same time, there’s a shortage of data on how new cancer therapies affect the population because clinical trials tend to enroll younger, physically fit patients who are better able to handle side effects and less likely to have other health conditions.
That has spurred Mohile to advocate for more clinical trials for the elderly, more collaboration among oncologists across the country, and more funding to disseminate and follow up on interventions used and recommended by the Wilmot clinic.
“Patients who fall or have a cognitive impairment are more likely to do poorly,” says Mohile, who is sponsoring a conference this spring on improving quality of life for older cancer survivors. “That’s not widely recognized, and we’ve added to the literature about that.”
The geriatric clinic has New York’s only outpatient geriatric assessment program for cancer patients. While physicians have long used a geriatric assessment survey to measure such things as function and mood, Wilmot adapted the survey for use with cancer patients, helping detect problems caused by the illness and tied more closely to survival rates.
Mohile hopes studying whether the model can reduce toxicity from chemotherapy in older adults, as well as whether it improves communication among patients, physicians, and caregivers, will lead to policy changes and lower health care costs.
Donald Walters, a retired engineer who was treated for stomach cancer in 2013, says Wilmot’s approach benefited him considerably. Hospitalized for nine days, and on a feeding tube for three weeks, Walters went through 26 weeks of radiation and 400 hours of chemotherapy.
As an octogenarian and because of the seriousness of his cancer, he was put on a five-year follow-up protocol involving medical tests every four months, physical therapy, and persistent reminders to keep active.
“I’m a person who doesn’t want to be pampered, but I had the greatest care all the time, every day,” Walters says. “It was like when you’re little and sick and home from school, and your mom keeps coming in to check on you. And that’s what gets you through it.”
“Targeted geriatric care” is critical given that between 60 and 70 percent of patients whom community oncologists are going to see will be older than 65, says William Dale, who established and helps direct the Specialized Oncology Care and Research in the Elderly Clinic at the University of Chicago.
His clinic is a site for both of Mohile’s grant-funded studies. Mohile “has the ability to go outside the standard networks to find the right people across the country and then coordinate with them to get data. She has put Rochester on the map when it comes to getting information about the patients we actually treat.”
Helping Survivors
Survivorship is a hot topic in the medical community, with conferences and research papers exploring innovative, evidence-based approaches for the physical and emotional care of cancer survivors.
Gary Morrow ’77 (Flw), ’88 (MS), the Benefactor Distinguished Professor, directs the Wilmot Cancer Institute’s Cancer Control and Survivorship research program.
As the principal investigator of an $18.6 million, five-year NCI grant, he’s leading a nationwide clinical research network in investigating cancer-related side effects.
The funding is the largest investigator-initiated grant at the University, and among the top five largest grants received by a Medical Center researcher in the past decade.
One of the first to treat nausea and vomiting as side effects of chemotherapy, Morrow and his team will design and manage clinical studies across the country that center on providing supportive, community-based care for patients coping with side effects both during and after cancer treatment.
Wilmot is one of only two cancer centers chosen by NCI as a research hub for its community-based cancer research program known as NCORP. In an effort to minimize or eliminate side effects from cancer treatment, the institute also leads hundreds of researchers in 22 affiliated research sites as part of NCI’s Community Clinical Oncology Program.
With a dual perspective as the top Wilmot administrator and a practicing physician, Friedberg says there is a solid link between his strategic planning goals and the insights he gains from the follow-up he provides beyond treatment.
“There’s no question my experience with patients has formed to some degree how we think about the institute moving forward,” he says. “I have had many patients who, fortunately, are cancer survivors, and I appreciate how many issues they still continue to have despite the fact that their cancer treatment is finished.”
To address such issues, Wilmot began the Judy DiMarzo Survivorship Program—the first in the region to assist patients as they cope with delayed or long-term physical and psychological effects after treatment. Nearly 300 patients have been enrolled in the program, and cancer programs nationwide call regularly for advice on beefing up their own approach to survivorship.
 GRATEFUL PATIENT: Jason Buitrago ’07, ’14W (MS) says the Wilmot staff helped him navigate the mental and emotional—as well as the physical—aspects of his treatment. (Photo: Adam Fenster)
GRATEFUL PATIENT: Jason Buitrago ’07, ’14W (MS) says the Wilmot staff helped him navigate the mental and emotional—as well as the physical—aspects of his treatment. (Photo: Adam Fenster)For Jason Buitrago ’07, ’14W (MS), who had 12 weeks of chemotherapy after a testicular cancer diagnosis last year, survival meant getting involved with support groups to help others the way Wilmot helped him.
“There’s so much out of your control as a patient, and I failed to realize initially that I was going to need resources to navigate the emotional and mental health challenges I encountered,” says Buitrago, who works as assistant director of IT and operations at the Simon Business School and is pursuing a doctorate at the Warner School of Education.
Leveraging Research through Collaboration
Last May, the University launched a four-year, $30 million fundraising campaign to recruit scientists and solidify a place among elite research centers in the country. As an integral part of the effort, Wilmot aligned itself with Buffalo’s Roswell Park Cancer Institute to amplify faculty recruitment efforts, funding, and the development of larger research studies.
Collaboration takes place within the institute as well. Consider that patients who have bone marrow transplants often bleed and require platelet transfusions after they have high doses of chemotherapy or radiation.
With assistance from the Department of Radiation Oncology and the Blood and Marrow Transplantation team, professor of medicine Jane Liesveld tested whether administering a particular post- transplant compound sped up platelet recovery time.
With the initial testing phase complete and published results that show the process is safe, Liesveld says “it looks like this is something that has the potential to be carried forward.”
Wilmot’s Samuel E. Durand Blood and Marrow Transplant Program is the state’s second largest.
Fighting Blood Cancers
When it comes to the most prevalent form of blood cancer in the United States, Wilmot is one of the few cancer centers in the nation, and the only one in upstate New York, that has a clinic focused on chronic lymphocytic leukemia.
In addition, former Wilmot director Richard Fisher played a major role in creating guidelines for lymphoma diagnosis and management. And John Bennett, professor emeritus of medicine, pathology, and laboratory medicine, was instrumental in the development of a classification system for leukemia used globally for nearly two decades.
Conducting Clinical Trials
Friedberg, the director of Hematological Malignancies Clinical Research, keeps Wilmot active as an executive committee member of NCI’s National Clinical Trials Network, which works to streamline clinical trials and boost participation rates.
For several years, Wilmot has led the country in the number of cancer patients who sign up for key clinical trials through a national cancer research cooperative group.
In 2013, more than 500 patients enrolled in 160 local and national trials.
Such trials led recently to FDA approval of two drugs to treat leukemia and lymphoma. One drug went through an accelerated approval process after trial participants showed significant improvement early on.
“What this means is that patients in our region are able to get drugs sometimes years before the Food and Drug Administration approves them,” says Friedberg.
Robin L. Flanigan is a Rochester-based freelance writer.