Features
 FOUNDER: As the School of Nursing’s founding dean, Loretta Ford led the program for more than a decade (above), helping to advance the role of nurse practitioner, a history that she recounted on campus this fall (below). (Photo: University Libraries/Department of Rare Books, Special Collections, and Preservation)
FOUNDER: As the School of Nursing’s founding dean, Loretta Ford led the program for more than a decade (above), helping to advance the role of nurse practitioner, a history that she recounted on campus this fall (below). (Photo: University Libraries/Department of Rare Books, Special Collections, and Preservation)As one of the few health care professionals serving a large section of mountainous and rural Colorado in the 1940s and ’50s, Loretta (Lee) Ford realized that she had to be a bit of a “Lone Ranger.”
Trained as a public health nurse, she was often the only source of care for children and families, making sure they received immunizations, checking in on nursing homes, collecting health statistics, and even testing wells.
 (Photo: Matt Wittmeyer for the School of Nursing)
(Photo: Matt Wittmeyer for the School of Nursing)“I was very used to being fairly independent in terms of my decisions, but I learned [how to do] that in the hospital,” Ford says.
When necessary, she consulted physicians, but by the 1960s, physicians, especially in rural areas, were becoming scarce.
“There was a shortage of physicians,” Ford says. “The shortage was a good thing because it gave us the opportunity to try something new.”
That new development turned out to change much of the face of health care during the past 50 years. In 1965, Ford, along with Henry Silver at the University of Colorado Medical Center, introduced the model of the nurse practitioner.
Connecting the patient-oriented focus of skilled nursing practice with advanced education in both clinical care and research, the new model of nursing professional was designed to better meet the needs of patients as well as allow nurses to practice to the full extent of their capabilities.
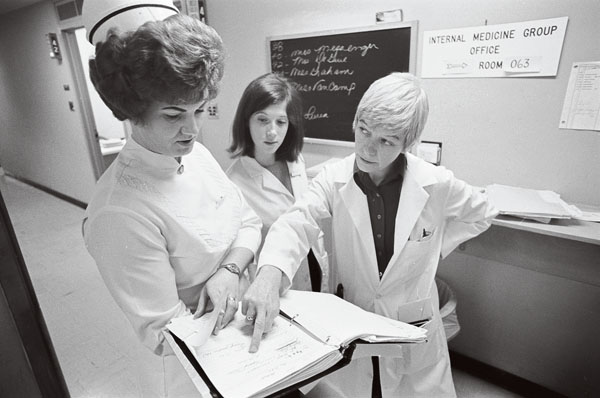 NEW MODEL: First introduced in 1965, the role of nurse practitioner brought together practice and education in a way that
has helped transform health care. (Photo: University Libraries/Department of Rare Books, Special Collections, and Preservation)
NEW MODEL: First introduced in 1965, the role of nurse practitioner brought together practice and education in a way that
has helped transform health care. (Photo: University Libraries/Department of Rare Books, Special Collections, and Preservation)Kathy Rideout ’95W (EdD), dean of the School of Nursing, says the idea helped transform the roles of nurses. “In that next level of care, you would have individuals who would assess, diagnose, treat, and manage patients in a variety of different settings and with a variety of different issues.”
When Ford was named the founding dean of the School of Nursing in 1972, she brought her forward-looking outlook for the profession, Rideout says.
“With her came her vision and her plans for what nursing could be, recognizing what it was and recognizing the strength within each one of us to move the profession in a whole different direction.”
The school celebrated the anniversary and Ford’s role in leading the transformation during a series of events this fall hosted by the Margaret D. Sovie Center for Advanced Practice. The center is named in recognition of the late Margaret Sovie, who as director of nursing at Strong Memorial Hospital worked with Ford to integrate advanced practice nursing into acute care. That approach, known as the unification model of education, practice, and research, changed how health care facilities support professional nursing practice.
“The marriage of education and practice was vital to nursing in Rochester,” Ford says. “Rochester had the philosophy and the interdisciplinary aspects to develop a team approach and establish a system that was receptive and responsive to new ideas.”
Today, there about 200,000 nurse practitioners in the United States. More than 400 nurse practitioners are employed at Strong Memorial Hospital, and the School of Nursing offers master’s programs that prepare nurse practitioners in six different specialties.
Julie Berkhof, regional clinical leader at Wilmot Cancer Institute and a graduate of the School of Nursing’s family nurse practitioner program, says she takes pride in being an integral part of the patient care team.
“Nurse practitioners make everything possible. To be a part of the patient story is huge, and if you interviewed any of the nurse practitioners here they would say that’s the best part of their job. It all flexes based on the needs of patients, first and foremost.”
As for Ford, she hopes members of the profession continue to challenge themselves to contribute in new ways to improving health care. As the landscape of care changes, whether that’s driven by federal policies, new technology, more personalized approaches, or advancements in data gathering, nurses must bring energy, imagination, and courage to their work, she says.
“We have opportunities for nurses to be innovative, to be inquiring, to ask some really tough questions.”

