Features
 FIRST TEAM: Kenneth DeHaven was “a one-man band,” he says, when he started Rochester’s sports medicine program under new orthopaedics chair C. McCollister (Mac) Evarts ’57M (MD), ’64M (Res) in 1975. By embracing and working to perfect promising experimental techniques, DeHaven put the program on the path to becoming a regional destination for athletes. (Photo: Adam Fenster)
FIRST TEAM: Kenneth DeHaven was “a one-man band,” he says, when he started Rochester’s sports medicine program under new orthopaedics chair C. McCollister (Mac) Evarts ’57M (MD), ’64M (Res) in 1975. By embracing and working to perfect promising experimental techniques, DeHaven put the program on the path to becoming a regional destination for athletes. (Photo: Adam Fenster)Only one University athlete has gone from the River Campus to a major sports team: Dave Deutsch ’66 played in just 19 games for the New York Knicks of the National Basketball Association. But in the world of sports medicine, Rochester has fielded an all-star lineup.
Kevin Black ’81M (MD) ’86M (Res) was orthopaedic consultant to the National Football League’s Green Bay Packers from 1990 to 1992 and since 1993 has been team physician for the American Hockey League’s Hershey Bears.
Jan Fronek ’78M (MD) was head team physician for Major League Baseball’s San Diego Padres (1991–2008), the U.S. Pro Ski Tour, and the World Baseball Classic, an event that brings together top players from 16 nations. Among his regular patients was Baseball Hall-of-Famer Tony Gwynn, who won eight National League batting championships despite eight knee surgeries.
Elliott Hershman ’75, ’79M (MD) is the team orthopaedist for the New York Jets, a position he’s held since 1991. He began working with the National Football League team in 1976 while still a medical student, and continued with the Jets while he as an orthopaedic resident at New York City’s Lenox Hill Hospital. He’s also served on the medical staffs of the NFL’s Cleveland Browns, the NBA’s Cleveland Cavaliers, and the New York Islanders of the National Hockey League. Now the chair of orthopaedic surgery at Lenox Hill, he also chairs an NFL panel on injury and safety.
Jim Malone ’89 served as head strength and conditioning coach for Major League Baseball’s San Diego Padres and New York Mets. He’s now the athletic development coordinator for the St. Louis Cardinals.
The late Arthur Pappas ’57M (MD) was medical director of the Boston Red Sox from 1978 to 2002. He was instrumental in prolonging the careers of several players, including Roger Clemens, who overcame shoulder surgery in 1984 and pitched until 2007, winning 354 games. Hall-of-Fame outfielder Carl Yastrzemski, who played until age 44 despite chronic back ailments, credited Pappas’s impact on his long career.
Wayne Sebastianelli ’79, ’83M (MD), ’88M (Res)was Penn State’s head physician from 1992 to 2013 and now serves as its director of athletic medicine. His quick work helped football player Adam Taliaferro recover from a spinal injury in 2000 after the freshman was given only a 3 percent chance of walking again. He walked eight months later.
Tommy Sheehan ’90 was Columbia University’s director of strength and conditioning from 2001 to 2014 and is now the director of sports performance at the Ivy League school. A two-time All-American wide receiver for the Rochester football team and a member of the University’s Athletic Hall of Fame, he has trained Cristina Teuscher, an Olympic gold medalist in swimming; Mahesh Bhupathi, a world champion in doubles tennis; and Alexei Kovalev, a National Hockey League All-Star for the Pittsburgh Penguins and Montreal Canadiens.
Bojan Zoric ’98 has helped some of the world’s greatest soccer players as a team doctor for the United States women’s national team during its gold medal–winning performance at the 2012 Olympics and championship win at the 2015 World Cup. (See story, page 33.)
In addition, a team of doctors at UR Medicine–Sports Medicine, led by division chief Mike Maloney ’97M (Res), helped pole vaulter Jenn Suhr recover from injuries and go on to win the gold medal in the 2012 Olympics. The Fredonia, New York, native finished second at the 2008 Olympic Games, but after injuries threatened to sideline her in 2012, Rochester doctors were able to relieve her pain and avoid surgery. She rose to No. 1 in the world rankings before capturing the gold in London.
“The URMC doctors got me back in action,” Suhr says. “I never could have done this without them.”
—Jim Mandelaro
The summer before her senior year of high school, Brynn Lauer ’17, her basketball team’s Most Valuable Player and a regional standout, endured one of the most dreaded injuries in sports: a tear in the anterior cruciate ligament in her right knee. The ligament—known as the ACL—sits at the center of the knee, stabilizing the entire joint.
“It’s a feeling I’ll never forget,” says the chemical engineering major from Newark, New York, outside of Rochester. “I can play that moment over and over in my mind with such clarity, it sends chills down my spine.”
Lauer underwent surgery and endured six months of physical therapy before getting back to the court. But shortly after her return, she tore her right ACL again. Five weeks later, she tore her left ACL.
Three tears, and three surgeries, in 12 months.
Lauer missed her freshman season at Rochester, but this daughter of a high school coach, valedictorian of her class at Newark High School, refused to quit. And last season, her knees covered in braces and wraps, Lauer led the Yellowjacket women to the quarterfinals of the NCAA Division III tournament, recording 105 assists and starting 26 games.
“Brynn has been our hardest worker since her arrival at UR,” women’s basketball coach Jim Scheible says. “She has worked her way back from three ACL tears to become our starting point guard and unquestioned leader. Her will to compete and her resiliency amazes the players and coaching staff on a daily basis.”
Lauer considers herself fortunate. Thirty years ago, an ACL tear could end a career. But medicine has come a long way since then. Reflecting on her treatment, Lauer says, “It has helped me get back on the court and feel as close as possible to my ‘normal’ self.”
At the heart of that medical progress is arthroscopic surgery: a minimally invasive procedure in which an endoscope is inserted into a damaged joint through a small incision. Hundreds of thousands of injured recreational and professional athletes have been able, like Lauer, to return to their “normal selves” because of what it’s been able to do for damaged knees, shoulders, elbows, wrists, ankles, feet, and hips.
Over 40 years, arthroscopy has transformed sports medicine from a minor branch of orthopaedics to a thriving field that has enhanced quality of life for patients and changed the way orthopaedists deliver care.
“From a patient’s perspective, sports medicine is one of the most sought-after types of orthopaedic care,” says Paul Rubery, chair of the orthopaedics department at the Medical Center. “From the surgeon’s perspective, it is probably the sub-specialty of our field which has had the greatest impact on changing what it means to be an orthopaedic surgeon in the past 40 years.”
The art of arthroscopy
Rochester was an early leader in the adoption of arthroscopy. One of the first physicians to recognize its potential was Kenneth DeHaven, professor emeritus of orthopaedics, who joined the Medical Center in 1975.
DeHaven had worked as an intern at the Cleveland Clinic with C. McCollister (Mac) Evarts ’57M (MD) ’64M (Res). Evarts left Cleveland in 1974 to return to Rochester and establish an orthopaedics department at the Medical Center. Eventually he would build the department into a nationally recognized center of orthopaedic treatment and research. One of his first steps in that transformation was to recruit DeHaven to become the University’s first director of athletic medicine.
“There weren’t many universities with a sports medicine department then,” DeHaven says. “Mac was ahead of the curve, and we had the blessing of the athletic director and coaches.”
When the two physicians were working together at the Cleveland Clinic, Evarts asked DeHaven what he wanted his career focus to be. “I said ‘arthroscopy,’ ’’ DeHaven recalls. The technique hadn’t been around for long. The first practical arthroscope—a thin, pencil-sized tube with a magnifying lens and light source—had been developed by Japanese orthopaedic surgeon Masaki Watanabe in the 1950s. A Canadian surgeon, Robert Jackson, visited Tokyo during the 1964 Summer Olympics, where he met Watanabe and brought the idea of modern arthroscopic techniques to North America.
Evarts supported DeHaven’s interest in the emerging technology. “He sent me to Toronto to learn under Dr. Jackson,” DeHaven says. “In Cleveland, we couldn’t see anything more inside the knee using an arthroscope than we could through an incision. But Jackson put the patient’s leg in a totally different position than we had been doing. He said, ‘Now look in there.’ And there it was. We could see so much more.”
When doctors had performed open knee surgery, it left patients with a six-inch scar, and often required a five-day hospital stay. Patients used crutches for three weeks and were fortunate to be running six months after surgery.
With arthroscopy, only two small incisions were made—one for the arthroscope and one for the surgical instruments used in the knee cavity. It was much less invasive, vastly reducing recovery time. It has improved greatly since. Surgeons now view the joint area on a video monitor and can diagnose and repair torn tissue in about one hour. A patient with a tear in the meniscus, the cartilage that cushions the knee joint, is often running within three weeks.
DeHaven couldn’t understand why there wasn’t more of an attempt to mend and salvage cartilage—and salvage an athlete’s career. He arrived in Rochester eager to spread the word about the groundbreaking technique. He appeared in hotel conference rooms from Rochester to San Francisco, representing the American Academy of Orthopaedic Surgeons and preaching the gospel about the advantages of arthroscopy versus traditional, more invasive open surgery.
But doctors weren’t buying what he was selling.
“They thought their way was best,” DeHaven says. “They thought arthroscopy was a fad.”
DeHaven persevered. At first “a one-man band,” with Evarts’s support, he made Rochester’s new sports medicine program a flourishing enterprise.
 INSTANT RE-PLAY: The Yellowjackets’ Brynn Lauer ’17 (above) plays with a knee brace, but has largely recovered from multiple ACL tears. UR Medicine–Sports Medicine’s Mike Maloney ’97M (Res) (below) confers with his patient, former Cornell football offensive lineman Matt Simmonds. (Photo: Jessica Hill/AP Images for Rochester Review)
INSTANT RE-PLAY: The Yellowjackets’ Brynn Lauer ’17 (above) plays with a knee brace, but has largely recovered from multiple ACL tears. UR Medicine–Sports Medicine’s Mike Maloney ’97M (Res) (below) confers with his patient, former Cornell football offensive lineman Matt Simmonds. (Photo: Jessica Hill/AP Images for Rochester Review)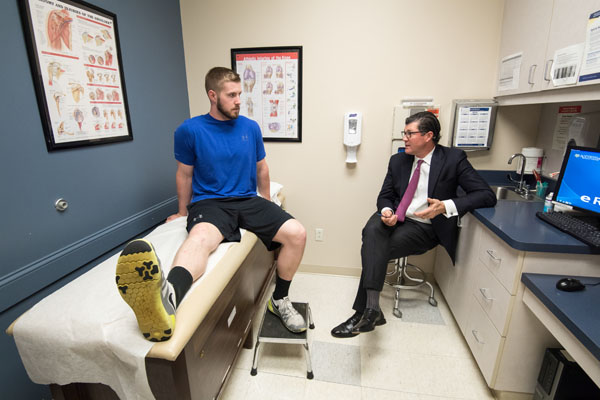 (Photo: Adam Fenster)
(Photo: Adam Fenster)More than 40 years later, it’s grown into UR Medicine-Sports Medicine, a team of doctors, technicians, therapists, and trainers numbering in the hundreds. Part of the Department of Orthopaedics and Rehabilitation, its lineup includes 10 physicians and 12 advanced practice providers who provide medical and surgical care, and 32 athletic trainers who deliver services such as classes in spine and knee injury prevention and nutrition consultations in four medical offices in Rochester and the surrounding area.
 SCARY MOMENT: U.S. women’s national soccer team physician Bojan Zoric (right) and athletic trainer Rick Guter attend to midfielder Morgan Brian after her head collided with that of an opposing team player in a 2015 World Cup semifinal game. (Photo: Jean-Yves Ahern/USA Today Sports)
SCARY MOMENT: U.S. women’s national soccer team physician Bojan Zoric (right) and athletic trainer Rick Guter attend to midfielder Morgan Brian after her head collided with that of an opposing team player in a 2015 World Cup semifinal game. (Photo: Jean-Yves Ahern/USA Today Sports)Bojan Zoric ’98 knew early on he wanted soccer to be part of his life: he was playing almost from the time he was walking. But it wasn’t until he suffered knee and foot injuries as a Rochester soccer player that Zoric developed an interest in sports medicine.
“Dr. Bronstein took care of me,” he recalls, referring to Robert Bronstein, the professor of orthopaedics at Rochester who treated Zoric in his clinical practice. “Watching him get me back on the field made me want to do the same for others. My injuries pushed me toward sports medicine.”
Zoric now practices at Sports Medicine North in Peabody, Massachusetts, where he specializes in sports medicine and arthroscopic reconstructive surgery of the hip, knee, shoulder, and elbow. He is also a team physician for the United States women’s national soccer team, which will enter this summer’s Olympic Games in Brazil ranked number one in the world.
Zoric will miss the Olympics, opting to stay home “for family reasons.”
“They’ll have to win gold without me,” he says with a laugh.
Zoric completed a sports medicine fellowship at the Steadman-Hawkins Sports Medicine Clinic in Vail, Colorado, where he worked with professional athletes from Major League Baseball, the National Football League, the National Basketball Association, the National Hockey League, and European soccer. He was also part of the team of physicians for the United States ski and snowboard teams.
Zoric was born at the University’s Strong Memorial Hospital while his father, Igor Zoric ’77 (PhD), was earning a doctoral degree in physics on the River Campus. He moved with his parents to their native Croatia when he was a year old, later lived in Sweden, and played for a youth club run by a professional soccer team until he was 18.
Igor wanted his son to have a college education and made contact with then Rochester soccer coach Mike Pilger, who recruited Bojan. Bojan majored in molecular biology and played four years of soccer. After overcoming a fifth metatarsal fracture and a meniscus tear, both requiring surgery, he was finally injury-free his senior year and tied for the team lead in scoring, with 18 points.
Zoric says that, among soccer players, injuries to the lower extremities are most common. He calls anterior cruciate ligament, or ACL, tears “a huge epidemic in the U.S. and around the world,” one that is growing with the increase in sports participation among youth.
“Kids are getting into athletics at a younger age, and with greater intensity,” he says. “There’s an unbelievable spike in ACL injuries among middle-school students, primarily girls.”
Zoric has been a leading proponent of programs focusing on prevention of ACL injuries, widely considered the most serious type of knee injury because of the ligament’s role in stabilizing the entire knee joint. Female athletes sustain noncontact tears at a rate five times higher than their male counterparts, largely as a result of different biomechanics. Female knees tend to be more turned in toward the middle of the body, and less bent when jumping and landing.
“There are several studies showing an increased incidence of ACL tears in females,” Zoric says. “This is thought to be multifactorial—biomechanics, hormonal, ligamentous laxity, et cetera. There’s also good evidence that going through a preseason strengthening exercise program which emphasizes mechanically correct landing techniques helps reduce the incidence of ACL tears in both men and women.”
Rochester’s sports medicine department implemented a program called PEP (Prevent injury, Enhance Performance) in 2003 at area high schools that targeted the prevention of noncontact ACL tears. It was based on a two-year clinical prevention trial among 1,400 Division I female college athletes showing that increased flexibility, strength, proprioception, and agility can reduce the injuries by up to 88 percent.
—Jim Mandelaro
Rochester has made a powerful impact on sports medicine through its graduates. John Bergfeld, senior surgeon in the Cleveland Clinic’s orthopaedics department and former team physician for the National Football League’s Cleveland Browns and National Basketball Association’s Cleveland Cavaliers, praises the breadth of Rochester’s sports medicine program. “Rochester has produced a wealth of sports physicians, not only at the professional and college athlete level, but also for schoolboy, schoolgirl, and recreational athletes,” he says.
Alumni include team doctors at Major League Baseball, NCAA Division I, and Olympic ranks, while UR Medicine–Sports Medicine has become an invaluable resource in the region, handling more than 75,000 patient visits per year from high school and college athletes and recreational golfers, skiers, tennis players, and exercise enthusiasts.
“I’m proud of what we have built, and how we serve the community,” says Mike Maloney ’97M (Res), professor of orthopaedics, chief of UR Medicine–Sports Medicine, and team doctor for the Triple-A baseball Rochester Red Wings. “It’s a tribute to what Dr. DeHaven started and envisioned for care of the athlete.”
The “Tommy John miracle”
Maloney followed a similar path to Rochester as did DeHaven. DeHaven has been highly attuned to recruiting other physicians on the forefront of novel techniques. In the late 1990s, he and Richard Burton, then chair of the orthopaedics department, brought Maloney to Rochester from the Kerlan-Jobe Orthopaedic Clinic in Los Angeles, where Maloney had learned a groundbreaking surgical technique from the late Frank Jobe, a pioneer in sports medicine who was the longtime team doctor for the Los Angeles Dodgers.
In 1974, Dodgers pitcher Tommy John sustained major damage to the ulnar collateral ligament in his left (throwing) elbow. Such an injury had ended pitchers’ careers in the past, but John pleaded with Jobe to fix it.
Jobe told John that he wasn’t sure he could, but he would try. Jobe had previously taken the palmaris longus, an “accessory” tendon in the forearm, to strengthen the joints of polio patients. He transferred the palmaris longus from John’s right forearm into his left elbow, weaving it through the tunnels drilled into the ulna and humerus bones.
Jobe gave John a 1 in 100 chance of recovery and warned that his elbow could snap at any time. It never did. John returned in 1976 and pitched 14 more seasons. Before the surgery, he had won 124 games. After it, he won 164. He never missed a start due to elbow pain and retired in 1989 at 46.
The experimental operation, formally called ulnar collateral ligament, or UCL, reconstruction, is known across baseball as “Tommy John surgery.” About 500 major league pitchers have undergone the surgery since 1974, and prospects of a complete recovery have risen to about 90 percent.
Having learned from the surgery’s inventor, Maloney quickly became a noted practitioner of UCL reconstruction. The number of cases can vary considerably, and Maloney estimates that he performs from 10 to 20 such surgeries in any given year. Outside of New York City, there are few physicians in the state, if any, who perform more.
Seeking the holy grail
Maloney marvels at the pace of change in sports medicine.
“I remember doctors saying ‘I did all this training, and there’s nothing I do now that I did when I trained,’’’ he says. “That speaks to our understanding of anatomy and the evolution of techniques in a minimally invasive way. It has changed the way we take care of patients.”
Although the strides made in sports medicine over the past half-century are staggering, there is more progress to be made. Maloney says Rochester doctors are investigating the use of platelet-rich plasma, or PRP, injections to promote the healing of injured tendons, ligaments, muscles, and joints.
Another strategy is harvesting stem cells from a person’s body, inserting them into the “defective” area, and sewing them in place with a piece of cartilage to see if a new layer of cartilage will develop.
“A lot of pro athletes are getting it done,” Maloney says. “We don’t have great prospective studies to say how well or how long it’s going to last, and for that reason a lot of insurance companies won’t cover it.”
Gene therapy, in which gene transfers are targeted to cartilage defects, is in the early stages.
“It’s had some complications,” Maloney says. “It’s just not there yet.”
A major area of research is on active citizens who are living much longer than in the past. “We’re talking about a population that once lived to 50 years old and now is living to 80, 90, and 100—but the joints aren’t lasting,” says Bojan Zoric ’98, physician for the United States women’s national soccer team (see story, above). “The holy grail is figuring out how to regenerate or restore cartilage in arthritic joints. And we’re still quite a ways from that.”
Maloney has treated hundreds of pro athletes whose livelihoods depend on their health. But perhaps his most challenging (and memorable) patient was a woman who insisted on knee surgery simply to continue her daily five-mile walks.
Never mind that she was in her early 90s.
“People told her to live with it, but she couldn’t,” he says. “So we did arthroscopic surgery and cleaned it up. She was so happy to get back to her walking.”
Maloney chuckles at the memory.
“You can help someone who is 9 or 90, and someone who makes millions playing sports, or one who just likes to work out,” he says. “That’s the beauty of sports medicine.”

