Features
They create novel devices that enable real-time biopsies, light the way for robotic surgery, and help independent-minded teens manage their asthma.
They develop new technologies to target the delivery of drug therapies with unprecedented accuracy, to help stroke victims regain their sight, and to vaccinate people with a simple, wearable skin patch that could reach global populations.
Lisa Beck, Danielle Benoit, Paula Doyle, Hyekyun Rhee, Krystel Huxlin, and Jannick Rolland: six women faculty members whose work spans the River Campus and the Medical Center. They’re among a growing group of women inventors at Rochester who are integral to the University’s success as a Tier I research institution.
According to a World Intellectual Property Organization survey of academic institutions worldwide, roughly half of Rochester-affiliated patent applicants are women, and the University ranked among the top five academic institutions in the United States, and top 40 worldwide, for the percentage of women patent applicants from 2011 to 2015.
Notably, women inventors are breaking through gender barriers not only in science but also in business. Rolland, the Brian J. Thompson Professor of Optical Engineering, is cofounder and chief technology officer of LightopTech. Doyle, an assistant professor of obstetrics and gynecology, is cofounder and chief medical officer of Endoglow.
Doyle praises colleagues who allowed her the flexibility to get Endoglow started. “Without their support I wouldn’t have been able to really pursue this,” she says.
“It is a whole different skill set being on the business side of things,” she adds. But it’s a role she’d like to see more medical professionals pursue.
“It shouldn’t be industry coming to us and saying, ‘Here, you need this.’ It should be the other way around, with doctors and nurses saying, ‘Hey, this is what we need; let’s develop it.’ ”
Jannick Rolland
Brian J. Thompson Professor of Optical Engineering
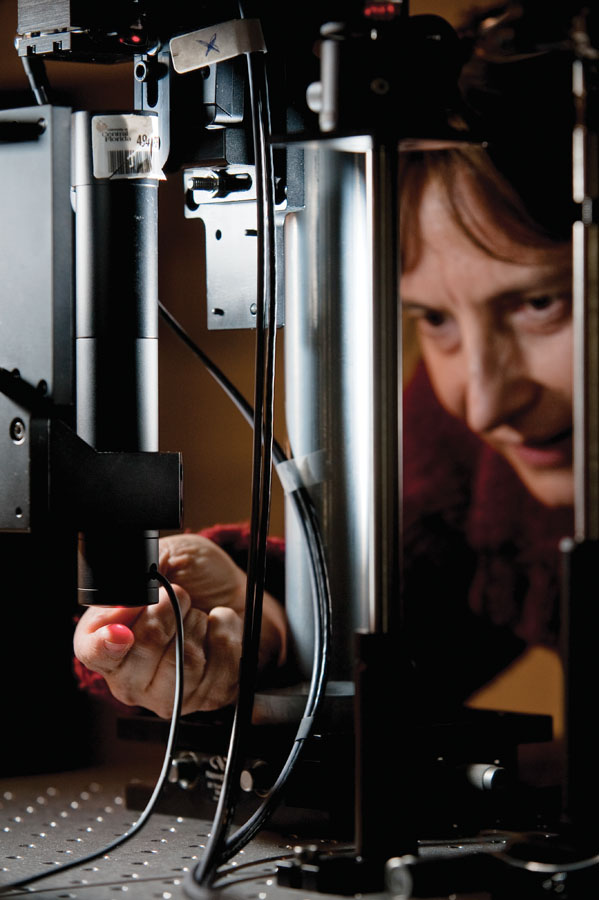 (Photo: J. Adam Fenster)
(Photo: J. Adam Fenster)After finishing as valedictorian in a two-year physics program at the Institut Universitaire de Technologie in Orsay, France, Jannick Rolland, who had once also been on the verge of a professional career in dance, remained in Orsay to enroll in a graduate program—the equivalent of a master’s degree—at the Institut D’Optique.
Then she set her sights on the United States.
She wanted to improve her English and applied to the University of Arizona’s distinguished optics program. But she was three points shy of passing Arizona’s required oral language exam.
She got on a plane anyway. After landing in Tucson, she marched to the admissions office and literally “talked her way” into the university. Within months she was being encouraged to join the PhD program in optical engineering.
The experience was eye opening. Some of the instruction at the Institut d’Optique had been “a little too much ‘push button’ for me,” Rolland says. “We were not encouraged to ask questions outside the box, just solve the problem in the typical way, just get the results.”
She experienced a far different approach at the University of Arizona’s Optical Sciences Center.
“I was surrounded by researchers who were very excited about what they were doing and really engaged in it,” Rolland says. “And the professors encouraged us to ask questions of all sorts.”
Rolland is now the Brian J. Thompson Professor of Optical Engineering at Rochester. She has 35 patents to her credit and has been listed among eight women pioneers in augmented and virtual reality by the organizers of the world’s largest AR/VR conference and expo.
She’s also the director of the Center for Freeform Optics, a federally supported collaboration involving Rochester, the University of North Carolina at Charlotte, and 18 companies and research institutes.
Freeform optics is an emerging technology that uses lenses and mirrors with freeform surfaces to create optical devices that are lighter, more compact, and more effective than ever before. According to Rolland, the technology “is poised to revolutionize instrumentation from space optics to microscopy.”
She adds that she was able to launch the center with the help of her colleagues and what she terms the strong “ecosystem” for biomedical development at Rochester.
That ecosystem is what helped her take the liquid lens technology, which she developed before she came to Rochester in 2009, and refine its biomedical applications.
Rolland and her former PhD student Cristina Canavesi have cofounded LightopTech, a startup commercializing one of Rolland’s inventions: a portable device that uses a microscope with a liquid lens to image cells just below the surface of the skin, cornea, and other tissues. Among many possible applications, the device is targeted to help surgeons determine if they’ve successfully removed all of a skin cancer, without having to wait for the results of a traditional biopsy.
She’s had her share of inspirational colleagues. But for the “first time in my life,” Rolland says, she finds herself surrounded by colleagues “who share common interests with me.”
 (Photo: J. Adam Fenster)
(Photo: J. Adam Fenster)Lisa Beck
Dean’s Professor, Department of Dermatology
Lisa Beck’s first research project—for AP biology in high school—took place in the basement of her family’s home in Portville, New York, a small town with “one stoplight,” she says.
From Portville, it was on to Mount Holyoke College, medical school at SUNY–Stony Brook, a residency at Rochester, and a faculty position at Johns Hopkins University, where she spent most of her 17 years there in the Division of Allergy.
In 2006, she returned to Rochester, where now, as Dean’s Professor in the Department of Dermatology, she’s led in the creation of a skin patch that could protect entire populations in hard-pressed developing countries against yellow fever, malaria, West Nile, Zika, and chikungunya.
The skin patch is based on two key discoveries rooted in Beck’s research on atopic dermatitis. The most common form of eczema, atopic dermatitis is a chronic skin disease that causes lesions, itching, and outright misery in its sufferers.
Beck and members of her lab discovered a defective protein that appears to be responsible for creating the “leaky” skin that causes the condition.
Leaky skin occurs when “water comes out, which makes the skin dry, and allergens, microbes, and irritants get in and cause the characteristic inflammation of the disease,” says Beck. Leaky skin provides an easy pathway for infection and disease.
In the meantime, Beck and her collaborators—Ben Miller, also a professor of dermatology, and Anna De Benedetto, formerly at Rochester, now associate professor of dermatology at the University of Florida—found a peptide that can temporarily “recreate” the same effect of having a faulty protein in healthy people as well.
That may not seem particularly helpful at first glance. But applied as part of a small wearable patch, the peptide can create temporary “leaks” in a very localized area of healthy skin. In doing so, it creates a perfect portal for vaccinating people as an alternative route for drug delivery.
The patch has worked in tissue cultures and in mice, thanks to the work of Matt Brewer, a postdoc in the Miller and Beck labs. “And the beauty of it is, when you remove the patch after 24 hours, the skin barrier recovers very nicely,” Beck says.
Think of it: vaccination without the burden of painful hypodermics, which require expensive biohazard disposal and highly trained health care workers.
A patent has been issued in the US, and others are pending overseas.
 (Photo: J. Adam Fenster)
(Photo: J. Adam Fenster)Hyekyun Rhee
Endowed Chair for Nursing Science and Professor of Nursing
When Hyekyun Rhee would meet teens with asthma, she’d often hear them wheeze and cough. When she asked them if they were OK, they’d say, “I’ve had this all my life, so I’m used to it.”
But Rhee knew she needed to come up with something—some process, some device—that would help teens better manage their asthma. Otherwise, the disease would continue to scar their lungs, turning healthy, flexible airways into rigid structures that would eventually cause far worse problems.
It would need to be something “cool” that would help teens overcome their sense of invulnerability and their reluctance to take their medications. Rhee decided to focus her research on asthma in part because her sister suffers from the condition. But she also “wanted to focus on something that affects a lot of teens.”
In her first faculty position, at the University of Virginia, she received funding for a peer-led asthma self-management program for teens. But it was hard to find enough teens to work with in Charlottesville. Rochester offered a larger population and pool of study participants—along with the prospect of collaborating with a senior investigator in the field. In 2007, she joined the faculty of the School of Nursing.
“Teens love technology,” Rhee says. And because most asthma symptoms are manifested in sounds, she came up with a novel idea: create a device that picks up those sounds, preferably in the form of an attractive pendant. It would connect to a mobile device that would then display the information, motivating teens to take medication to manage their symptoms.
Rhee found a collaborator across the street on the River Campus—Mark Bocko, Distinguished Professor of Electrical and Computer Engineering and chair of the department—whose lab developed algorithms to recognize the signature of a wheeze or cough. “Initially, we used an iPod for the detection and display of the symptoms,” Rhee says. Then, the technology was patented and licensed to Health Care Originals, which has modified the technology into a free-standing mobile device that can detect asthma symptoms along with other vital signs such as heart rate, respiratory rate, and body temperature.
But Rhee’s work isn’t over yet. A feasibility study has shown that the device works and that “teens and parents love it,” Rhee says. But clinical trials are necessary to determine whether its use will actually compel teens to manage their asthma, and thus improve their symptoms. Calling the technology “my baby,” Rhee says she’s gearing up to conduct those trials.
 (Photo: J. Adam Fenster)
(Photo: J. Adam Fenster)Paula Doyle
Assistant Professor of Obstetrics and Gynecology
After five years in fashion design, working as a top assistant for Paris Collections, Paula Doyle decided it was time for a change. “If the world suddenly dissolved, would you really care what designer pants you were wearing?” she asks.
She decided to pursue a medical career. And today, her willingness to embrace new challenges, to abruptly switch course along a career path that has been “to the left and right, and up and down,” is why she is a surgeon, inventor, and chief medical officer of a startup company.
Doyle arrived at Rochester for a three-year fellowship in urogynecology, treating female urinary incontinence and pelvic floor dysfunction. She found herself doing surgery by robot. “It’s like a video game,” she says. “You can control the robot with your hands, and when you look at the screen, the optics are really, really good—but you can’t actually feel what you’re operating on.”
During one surgery, Doyle needed to peel a bladder from scar tissue it was sitting on. It took a long time to finally figure out where to start. At a meeting of other fellows and their faculty mentors, she described how difficult the case had been and commented, “I wish I had a flashlight or something I could insert so I could see better.” Ron Wood and Jay Reeder, both research professors in obstetrics and gynecology, seized on the idea, and soon Wood, Reeder, and Doyle began “hashing out ideas” to turn her “complaint” into a viable prototype.
At the same time that Doyle completed her fellowship and joined the University as a surgeon and assistant professor, the problem she had identified in the operating room had resulted in a patented device called the GreenEgg. It is a small disposable device that uses a fluorescing polymer that can illuminate internal anatomy when near-infrared light is also used. For example, it provides backlighting that allows surgeons to see scarring and other pathologies deeper in the tissue than expected.
With the support of her supervisors, Doyle is working part time as an assistant professor, so she can spend more time as chief medical officer of Endoglow, the startup she and Reeder cofounded.
To her, her role in the company is a natural outgrowth of her physician’s role—and a type of function more physicians should consider performing.
“I really do believe in women’s health,” Doyle says, “and I think that physicians should be the ones to initiate progress, whether it’s in drugs or medical devices. It shouldn’t be industry coming to us and saying, ‘Here, you need this.’ It should be the other way around, with doctors and nurses saying, ‘Hey, this is what we need; let’s develop it.’ It should be inside out, not outside in.”
 (Photo: J. Adam Fenster)
(Photo: J. Adam Fenster)Danielle Benoit
Associate Professor of Biomedical Engineering
Danielle Benoit says she was “always tinkering” as a kid growing up in Maine. She remembers tagging along at work with her father, a forester who worked essentially as a civil engineer, designing remote logging roads for his company. “I remember all the survey equipment and other gadgets he had. I thought that was really cool,” she says.
Benoit became the first student to graduate in bioengineering from the University of Maine and went on to earn a PhD in chemical engineering at the University of Colorado. As a postdoctoral researcher at the University of Washington, she developed a delivery system for nucleic acid drugs used in cancer therapy.
Rochester sought to recruit her—and did so successfully in 2010. Benoit says the close proximity of the Medical Center to the biomedical engineering department was “critical” in her decision to accept a faculty position in biomedical engineering. So, too, was the number of women in the department.
“It wasn’t just women who were junior faculty members, but women who were senior and very well established, and who had thriving research programs,” she says.
Before joining the department, she had already met with Edward Puzas, the Donald and Mary Clark Professor in Orthopaedics at the Medical Center and an expert in bone remodeling. Puzas pursued exactly the kind of basic science research that could help her advance her work in tissue regeneration as well as the targeted delivery of therapeutic drugs that she began as a postdoc.
Puzas had discovered “a fantastic way to target bone drug delivery to exactly where it’s needed,” Benoit says. Working with Puzas, she and members of her lab began to design a nanoparticle-sized polymer drug-delivery device that could be loaded with therapeutic drugs to enhance the bone rebuilding process—in the case of a fracture—or to boost the performance of cells that aid in bone formation—in the case of osteoporosis or chronic bone thinning.
The result was US Patent #9,949,950: “Compositions and Methods for Controlled Localized Delivery of Bone Forming Therapeutic Agents,” one of nine approved or pending patents Benoit has coauthored.
Benoit is dedicated to schooling her students—the PhD students in her lab as well as more than 80 undergraduates she has mentored since arriving at Rochester—in how to disclose technologies developed in an academic lab and how to secure patents for them. “That’s critical, if we want to see what we have developed become a product that’s going to help people,” she says. “It’s going to take an investment in safety and efficacy studies and clinical trials, and so much development that is beyond the scope of what we can do in our labs.”
 (Photo: J. Adam Fenster)
(Photo: J. Adam Fenster)Krystel Huxlin
James V. Aquavella, M.D. Professor in Ophthalmology
When Krystel Huxlin arrived at Rochester in 1995, she intended to stay only two years.
Born in Romania, she had grown up in Europe and in Australia, where she studied neuroscience at the University of Sydney with pioneering vision scientist Ann Sefton. She culminated her studies with a prestigious, four-year early career fellowship, which allowed her to spend the first two years overseas.
Huxlin chose Rochester, where she studied with William Merigan and Tatiana Pasternak, professors of ophthalmology, neurobiology, and anatomy and both long-standing members of the Center for Visual Science. Meanwhile, she met Keith Nehrke ’94, now her husband and a professor of medicine in the Nephrology Unit. She decided to forfeit the last two years of her fellowship and stay at Rochester—not to abandon a career but rather to thrive in one.
“As a new faculty member in the Flaum Eye Institute, I became plugged in immediately with the Center for Visual Science, which has been vital to me and my work,” says Huxlin, who is now the James V. Aquavella, M.D. Professor in Ophthalmology.
Her research is helping stroke survivors who have suffered vision loss and promises better treatments for myopia patients worldwide.
For stroke victims, she has developed a “physical therapy” for the visual system. A set of exercises that stimulates use of visual information by undamaged portions of the visual cortical system, it helps the visual system relearn to interpret signals from a blind zone. The technology has been patented and licensed to Envision Solutions, which is running a three-site clinical trial with the technology.
Huxlin is also collaborating with Gabriel Diaz’s PerForM Lab at nearby Rochester Institute of Technology to develop virtual reality headsets with integrated eye tracking that patients can use at home—rendering in-home, long-term therapy as effective as that performed in Huxlin’s lab.
And working with colleagues at the Center for Visual Science, she’s helping to improve Lasik surgery, potentially transforming the way human vision is corrected. Her insights were instrumental in developing a technology, now licensed to the startup Clerio Vision, that will lead to individually customized vision corrections not only in contact and intraocular lenses but also directly into patients’ corneas. Critically, it can accomplish the task without having to cut eye tissue, as current Lasik surgery requires, a factor that prevents many people from electing to have the procedure.
“This technology could totally revolutionize the approach and feasibility of laser refractive correction,” she says. “And considering the myopia epidemic that is developing worldwide, it is not a moment too soon.”

