|
|
|
|
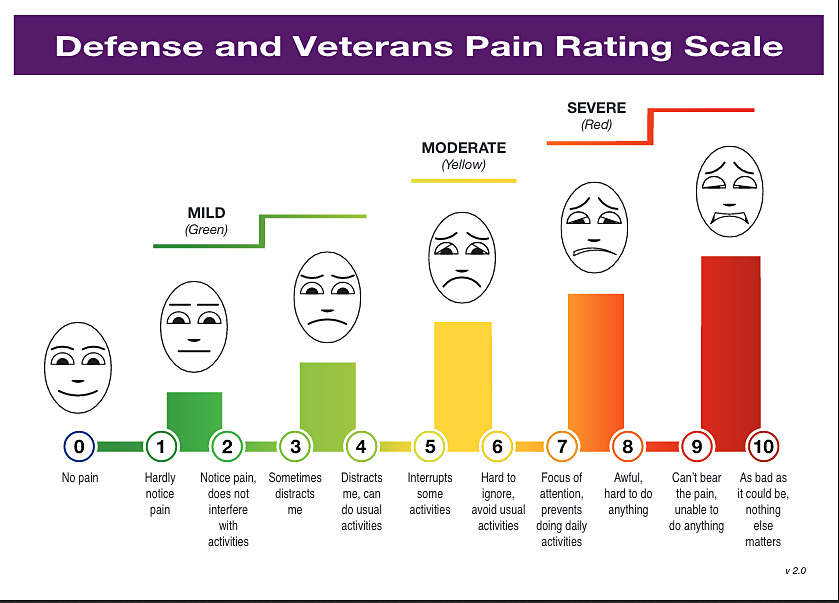 A pain scale from the Defense and Veterans Center for Integrative Pain Management incorporates several cues in an attempt to make the typical 0-10 pain rating scale easier to use and understand for patients in a clinical setting. However, in a clinical drug trial, the faces and the activity-related descriptions with each number would not be used, says Shannon Smith, assistant professor of anesthesiology. “The FDA wants to know how the drug being tested affects pain intensity, not its relationship to a participant’s activities and emotions.”
How patients rate their pain poses a challenge in clinical trials“Rate your pain on a scale of 0 to 10, with 0 being ‘no pain’ and 10 being ‘worst possible pain.’ ”
That request can be an efficient way for a nurse or doctor to quickly assess a patient’s pain level in an exam room.
But it can be problematic to ask that question both in clinical care and in clinical research because the contextual details that patients need to accurately rate their pain are not included. For example, what time period should be considered, and should the rating include all pains experienced or just the pain associated with a specific condition?
“If I am someone with osteoarthritis, the pain in my knee may be an 8 when I get up in the morning, but once I start moving around the pain lessens, and may be only a 3 later in the day,” says Shannon Smith, an assistant professor of anesthesiology. “So what are we asking that person to rate: their worst pain of the day, their ‘average’ pain for the day, or the pain they feel right now?”
When Smith and her colleagues reviewed clinical trial literature, it was not at all clear that the instructions given to clinical trial participants consistently address these kinds of questions. “If participants in these trials are not thinking systematically about their pain intensity,” Smith says, “we’re never going to know if the treatment we are testing works or not.”
Smith is attempting to meet this challenge as part of a $4 million FDA grant received by ACTTION (Analgesic, Anesthetic, and Addiction Clinical Trial Translations, Innovations, Opportunities, and Networks). The public-private partnership, directed by Robert Dworkin, professor of anesthesiology, received the funding to speed the discovery and development of analgesic, anesthetic, addiction, and peripheral neuropathy treatments for patients.
Other efforts have attempted to improve upon the 0-10 pain rating scale, such as the recently developed Defense and Veteran’s Pain Rating Scale (pictured above), which asks patients in clinical care settings to consider their pain intensity, level of functioning, and emotions when rating their pain.
However, in clinical trials to evaluate whether a drug should obtain FDA approval for use as an analgesic, the pain scale must solely measure pain intensity. Smith plans a two-step approach to developing a pain scale that elicits more accurate ratings:
- Getting feedback from patients on the three pain rating scales most widely used in clinical trials — two variants of the 0-10 scale, and a simple verbal rating of “none,” “mild,” “moderate,” or “severe.” How do patients interpret these scales and how do they use them to rate their pain? How could the scales be improved? Are there examples of pain that would be widely accepted by patients as a 1 or as a 10, to help “anchor” the outer parameters of the scales?
- Improving the instructions that clinical trial participants receive when being asked to rate their pain.
For example, research suggests that when people are asked to rate their “average” pain for a 24-hour period, the result could be biased. “People may readily remember their worst pain that day, and they’ll know what it is now, and then base their rating on those two experiences alone,” Smith says. Or they might rely on the “typical” pain they experienced even before their participation in the trial, irrespective of any improvements they might now be experiencing.
It might be better to avoid the word “average” altogether, and instead ask patients to think about how they felt at various stages of the day, Smith says.
Asking study participants to actually record their pain several times a day, on the other hand, could be viewed as burdensome over a typical 12-week trial for treatments for chronic pain, Smith says.
“Recruitment and retention for these trials is very difficult as it is. It’s a balance you have to strike. Perhaps we will find that simply providing patients with consistent instructions and systematic training will be all that is necessary to improve the accuracy of pain intensity ratings.”
$1 million gift supports research at School of NursingAn anonymous donor has pledged to give $1 million to the School of Nursing. The donation, which will establish a new endowed fund, will support the school’s mission to advance research and scientific discovery.
“This inspiring gift will allow us to embark on new research initiatives that have the potential to improve patient outcomes and address health care’s biggest challenges,” said Kathy Rideout, dean of the school. “We are immensely grateful for this donor’s generosity, which will have a lasting impact beyond our school and community.”
The endowed fund will provide resources to jump start new pilot projects, purchase state-of-the-art equipment, and conduct bio-statistical analysis, among other initiatives. The donation may also fund collaborative research projects led by the school and the School of Medicine and Dentistry.
Advancing research is one of the three core missions of the School of Nursing. Its faculty members have made significant contributions to research on promoting healthy behaviors, developing and changing health care systems, chronic illness and palliative care, and symptom identification, monitoring, and management.
In 2015, the school climbed 10 spots to No. 25 in the annual rankings of research funding from the National Institutes of Health — demonstrating the strength of the school’s research program in an increasingly competitive funding environment.
School of Nursing researchers identify possible target for dementia preventionA School of Nursing study has found that older adults with excellent memories have more efficient connections between specific areas of the brain — findings that could hold promise for the prevention of dementia and cognitive decline.
Although researchers have historically viewed memory deterioration as an inevitable part of the aging process, a small group of older adults — called “supernormals” — are able to maintain their memory capacities much better than their peers.
In a study published in Cortex, Feng (Vankee) Lin, an assistant professor at the School of Nursing, and her team explored differences in brain function among supernormals, older adults diagnosed with amnestic mild cognitive impairment who are at high risk for developing Alzheimer’s disease, and a healthy control group of older adults. The study is the first to compare the brain function of supernormals to those who are at risk for developing Alzheimer’s.
Specifically, Lin and her colleagues measured the functional connectivity between the cingulate cortex and other regions of the brain.
“The cingulate cortex acts as a ‘hub’ and receives input from many areas in the brain. Its functioning often deteriorates early in the aging process and in the development of Alzheimer’s disease, so it could play a key role in memory decline,” said Lin. “It’s a vulnerable area that hasn’t been explored in this way before.”
Lin found that individuals who had stronger or more efficient functional connectivity between the cingulate cortex and certain regions of the brain had better memories compared to those who had weaker or less efficient relationships between the same areas.
Supernormals also had lower levels of amyloids, groups of proteins that are associated with Alzheimer’s disease. But even when amyloids were present, the relationship between better functional connectivity and better memory still remained. These findings indicate that the way the cingulate cortex functions in supernormals may represent exceptional neural reserve — the ability of the mind to resist damage. This neural reserve could protect supernormals against the effects of amyloid plaques and allow their memories to be maintained.
“Our results show that the cingulate cortex could be a viable target for interventions aimed at preventing memory decline or enhancing memory capacity,” said Lin. “In the future, we may be able to modify the function of this region in individuals who are at risk for developing Alzheimer’s to slow down cognitive decline.” Read more here.
Collaboration improves understanding of developmental lung immunologyA decade-long collaboration between two University researchers has resulted in many publications, funding, and advances in our understanding of the developmental origins of lung disease.
In a Pediatric Research Newsletter story by Meghan Plog, Michael O’Reilly, professor of pediatrics, and Paige Lawrence, professor of environmental medicine, say they bring overlapping interests, but also differing perspectives to their collaboration. “We have a different toolbox, but it’s not so different that we don’t understand each other’s toolboxes,” said Lawrence. O’Reilly added, “She’s not asking me to come out of my area of interest and I’m not asking her to come out of hers, so it’s the perfect Venn diagram.”
O’Reilly is a development lung biologist who is interested in understanding how oxygen therapy given to preterm babies affects lung function later in life. Lawrence is an immunologist and toxicologist who studies how environmental factors have positive and negative effects on immune system development and function.
Initially, these investigators collaborated on a study in which mice were exposed to increased levels of oxygen at birth. Once the mice reached adulthood, they were infected with influenza virus. The oxygen-exposed mice developed significant interstitial lung disease. In contrast, injection of the virus into non-lung tissues led to a normal immune response and no interstitial lung disease. They concluded that early life oxygen exposure affects the programming of the lung and its ability to mount a normal immune response to infection.
To continue to explore these provocative findings, they recently submitted a grant application to study the expansion of a population of cells in the lung that may be responsible for the disrupted host response to respiratory viral infections. The long-term goal for the project is to identify a target that could be amenable to drug development. This work also involves collaboration with Luis Martinez-Sobrido, associate professor of microbiology and immunology.
In addition, Lawrence and O’Reilly plan to collaborate on studies of the aryl hydrocarbon receptor, a protein that binds hundreds of environmental factors and has an extremely important role in the immune system. Recently obtained data suggest that it also has an important role in the lung. Importantly, the role of aryl hydrocarbon receptor in the lung has not been extensively investigated.
Congratulations to . . .Ehsan Hoque, an assistant professor of computer science, who has been recognized as a leading innovator in human-computer interaction with a World Technology Award from the World Technology Network. Hoque applies a computational lens to understand and model the ambiguity that language, facial expressions, gestures, and intonation introduce in human communication. He has developed a system that allows individuals to practice speaking and social skills and receive feedback in a repeatable, objective, and respectful way. He has also developed systems that help singers practice vowels and provide live feedback to public speakers while they’re engaged with audiences. Read more here.
Kevin Parker, the William F. May Professor and dean emeritus of engineering, who has been named a fellow of the National Academy of Inventors. Parker’s discoveries have included Blue Noise Mask, a widely adopted half-toning technique that prints shades of gray in less time and at a higher quality than traditional methods; a series of patents that helped launch the field of sonoelastography; and, more recently, a technology that uses color coding to reveal fine details that have previously been obscured in ultrasound images. Read more here.
Introducing a new faculty memberAnna Rosensweig has joined the Department of Modern Languages and Culture as an assistant professor of French, after a two-year fellowship as a Provost’s Postdoctoral Scholar at the University of Southern California. Her scholarship and teaching focus on early modern literature and culture, the intersections of literature and political theory, and performance studies. She is currently completing a book manuscript, Tragic Opposition: Rights of Resistance on the Early Modern Stage, in which she locates a new genealogy of rights in early modern tragedy. She received her PhD from the University of Minnesota.
PI Oversight: Review of IRB approval letters(This is part of a monthly series to help principal investigators understand their role in ensuring that human subject protection requirements are met in their studies.)
Once Institutional Review Board (IRB) approval is obtained for a new study, an amendment, or a reapproval, study teams often rush to implement the approved procedures without taking the time to read the information provided within the approval letter. Each approval letter includes valuable information directly related to the conduct of your research study, including:
- Approval period – IRBs typically approve research studies for 1 year but the period can be shorter based on the nature of the research;
- Risk level – The risk level assigned to a study can affect the RSRB requirements of approval. For example, the informed consent process and the type of human subject protection training required;
- Regulatory findings & determinations – Determinations can include requirements concerning HIPAA authorization, informed consent, research information stored/identified in the electronic health record, investigational product storage/maintenance, or other approval contingencies;
- General expectations concerning roles and responsibilities, compliance, informed consent, event reporting, and study documentation.
Have a question about the information provided in your approval letter? Contact your reviewing IRB (local questions pertaining to the Research Subjects Review Board can be directed to your RSRB Specialist).
PhD dissertation defenseChitralekha Basu, Political Science, “Party Competition and Voter Priorities in Multi-Issue Contexts.” 3 p.m., December 16, 2016. Harkness 112. Advisor: G. Bingham Powell.
John Serafini, Physics, “Ultrafast Optical and Electronic Characterization of (Cd,Mg) Te Single Crystals.” 2:30 p.m., December 21, 2016. Bausch and Lomb 372. Advisor: Roman Sobolewski.
A break for the holidaysThe next issue of Research Connections will be January 6, 2017.
Mark your calendarToday: AS&E workshop for new and junior faculty on applying for NSF grants. 9 a.m. to 11:30 a.m., Gamble Room, Rush Rhees Library.
Today: Center for Integrated Research Computing symposium, 11:30 a.m. to 1 p.m., URMC 3-6408 (K-307 Auditorium). Tong Tong Wu from the Department of Biostatistics and Computational Biology will demonstrate the application of two-stage design in survival studies with small intestine cancer data. Emerson Khost from the Department of Biology will discuss a technique to resolve the detailed structure of complex satellite DNA loci.
Today: Meeting of the Junior Women Research Faculty Group. Noon to 1:30 p.m., Louise Slaughter Room (1-9555). Catherine Cerulli, director of the Laboratory of Interpersonal Violence and Victimization, will address the steps to creating and executing a research-focused Academic Development Plan (ADP). Please RSVP to Grace Fuller. A light lunch will be provided.
Dec. 21: Deadline to apply for Center for AIDS Research funding for focused pilot and research projects using the CFAR Pharmacology Shared Resource to address key gaps in the understanding of HIV/AIDS pharmacology and therapeutics. Additional information and specific application requirements can be found here.
Dec. 30: Deadline to submit proposals for two Breast Cancer Coalition research grants, one a maximum of $25,000 for pre- and post-doctoral trainee/fellows and the other $50,000 for faculty applicants. Click here for the full RFP.
Jan. 4: SCORE study group meets 4 to 6 p.m. to study for clinical research certification exam. If interested in participating, email SCORE@urmc.rochester.edu
Jan. 9: Ninth annual Lung Research and Trainee Day. Poster session in Flaum Atrium from 10 a.m. to noon. Keynote presentation by Enid Neptune, associate professor of medicine at Johns Hopkins University School of Medicine, “Lessons from the Marfan Lung: TGFbeta, Angiotensin and Lung Repair” at noon in the Class of ’62 Auditorium (1-9576). Boxed lunches will be provided.
Jan. 10: Deadline to apply for Schomburg-Mellon Humanities Summer Institute, a seven-week session for 10 rising seniors on the theme “The Global Black Experience in the 20th and 21st Centuries.” Click here for more information.
Jan. 31: Deadline to enter “America’s Got Regulatory Science Talent” competition, promoting student interest in the science of developing new tools, standards, and approaches to assess the safety, efficacy, quality, and performance of FDA-regulated products. Click here for information and instructions on how to apply.
March 20: Deadline to submit applications for a University Research Award of up to $37,500, matched by the applicant’s home school for a total of $75,000. The program provides seed money on a competitive basis for innovative research projects that are likely to obtain external support. Completed applications should be directed to Adele Coelho, faculty outreach coordinator in the Office of the Provost and Senior Vice President for Research, at adele.coelho@rochester.edu. Click here to view the full RFP.
|
|
|
|
|