|
|
|
|
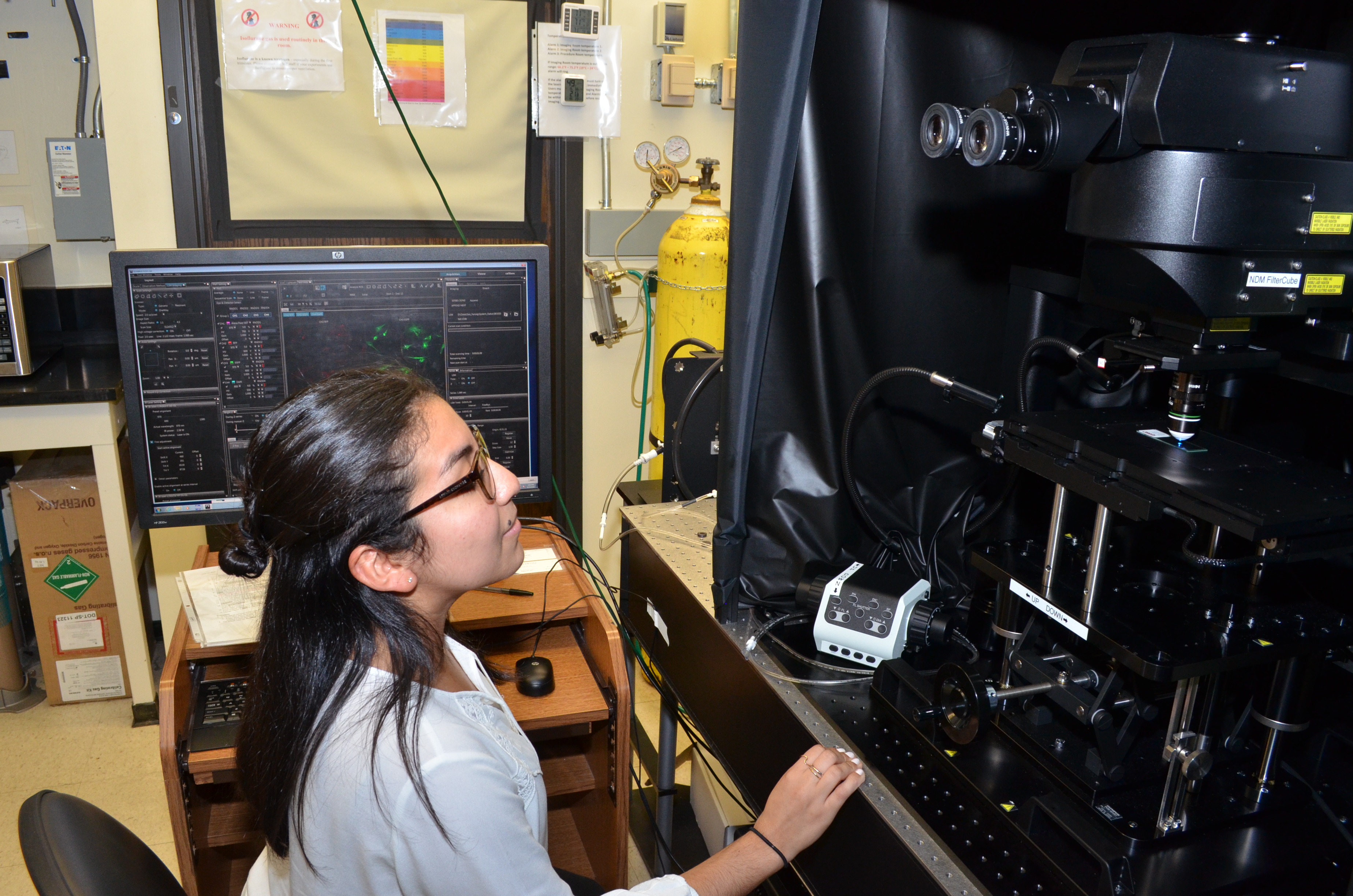 Emily Palachio, a laboratory technician in the Multiphoton Research Core Facility, with the Olympus Fluoview FVMPE-RS Twin Lasers Imaging System acquired in January.
New at the Shared Resource Laboratories: Two-photon microscopy(The Shared Resource Laboratories (SRL) have invested $3 million in the last year in new state-of-the-art instrumentation. These advanced technologies will enhance the University’s research capabilities in microscopy, mass spectrometry, genomics, and flow cytometry. This is the first in a series on the new instrumentation.)
The Multiphoton Research Core Facility is now equipped with an Olympus Fluoview FVMPE-RS Twin Lasers Imaging System, which was installed in January. This system was brought to the URMC, in part, with support from a NIH supplement secured by Deborah Fowell, professor of microbiology and immunology.
Two-photon laser scanning microscopy is a fluorescence imaging technique that uses near-infrared excitation light to achieve living tissue deep imaging.
The Multiphoton Core Facility provides University researchers the ability and expertise to obtain high quality imaging-based data from in-vitro tissue and intravital animal research studies in the fields of immunology, neuroscience, biomaterial engineering, biophysics, and cancer research.
Staff members within the laboratory have expertise in sample preparation methodologies and image analyses to support additional research needs.
(The Shared Resource Laboratories, which are directed by Tim Bushnell, provide leading edge services and instrumentation to researchers across the University. The new acquisitions were made possible through a combination of internal investment, NIH grant supplements, and NIH SIG grants.)
Blood test will help diagnose brain injuryFor the first time in the U.S., a blood test will be available to help doctors determine if people who’ve experienced a blow to the head could have a traumatic brain injury such as brain bleeding or bruising. Called the Banyan Brain Trauma Indicator®, the test aids in the evaluation of patients with a suspected traumatic brain injury or concussion, also known as a mild traumatic brain injury.
The results of a major clinical trial that led to approval of the test, just published in The Lancet Neurology, included close to 2,000 individuals presenting with a head injury to 22 emergency departments in the U.S. and Europe.
“Many concussion patients don’t seek medical care for their injury, a decision due in part to the perception that emergency departments have nothing to offer in terms of diagnosis,” said lead study author Jeffrey J. Bazarian, professor of emergency medicine at the Medical Center. “The results of this study show that we now have something to offer—a brain biomarker blood test. The ability of this test to predict traumatic injuries on head CT scan will soon allow emergency physicians to provide patients with an unbiased report on the status of their brain.”
The test detects two brain proteins that are present in the blood soon after a hit to the head. The new study shows that if the test is negative – meaning the brain proteins aren’t present – it is highly unlikely that a traumatic intracranial injury exists; therefore, a head CT scan can be safely avoided. If the test is positive, a brain injury may be present and the patient should receive a head CT scan to further assess the damage and guide treatment.
Approved for use in individuals 18 years and older, the test has the potential to reduce CT scans and the radiation exposure that comes with them. The scans are commonly used to evaluate brain injuries, but research shows that less than 10 percent of head CTs show any injury. Limiting scans to patients with a positive blood test could eliminate needless radiation, allow people to get in and out of the emergency room faster, and lower health care costs.
Read more here.
Congratulations to . . .Sally Norton, the Independence Chair in Nursing and Palliative Care at the School of Nursing, who has been honored with the prestigious Distinguished Researcher Award from the Hospice & Palliative Nurses Association (HPNA). The award recognizes nurse researchers who have made significant contributions to the science, allowing the specialty of palliative nursing to evolve and mature. Norton has successfully worked across professions to improve communication and understand the systems surrounding palliative care and hospice delivery in order to pinpoint the approaches most meaningful to patients and families, leading to the highest quality outcomes. Over the past two decades, she has played a role in dozens of funded research studies on palliative care and has authored (or co-authored) more than 70 papers. Read more here.
PI oversight: Protections against coercion or undue influence(This is part of a monthly series to help principal investigators understand their role in ensuring that human subject protection requirements are met in their studies.)
Department of Health and Human Service and Food and Drug Administration regulations (45 CFR 46; 21 CFR 56) define specific criteria that human subject research must meet in order for an Institutional Review Board (IRB) to approve the research. A critical, yet often overlooked step in the protocol development process is to objectively evaluate study protocols against these criteria prior to IRB submission. Doing so will help facilitate IRB review of the proposal, with the intent of minimizing IRB stipulations.
This month we look at approval criteria #8: “when some or all of the subjects are likely to be vulnerable to coercion or undue influence…additional safeguards have been included in the study to protect the rights and welfare of these subjects.”
Subjects who may be unable to adequately protect their own interests for any reason are generally considered to be vulnerable. Human subject protection regulations specifically identify children, pregnant women/fetuses, and prisoners as vulnerable populations, though Institutional Review Boards routinely recognize additional populations as vulnerable. This includes (but is not limited to) adults with decisional impairment, students, employees, economically disadvantaged persons, the elderly, and terminally ill patients.
In evaluating this criterion, the IRB will consider:
- Is the inclusion of the vulnerable population warranted?
- Are there additional measures needed to protect subjects in terms of the recruitment or informed consent process; where, how, or when study procedures occur; how privacy and confidentiality will be handled; subject payment processes; or methods of subject communication?
- If children, pregnant women/fetuses, prisoners or adults with decisional impairment will be recruited, have applicable regulations and OHSP policy requirements been met?
For previously highlighted criteria for IRB approval, see the 11/10/2017, 1/5/2018, 2/9/2018, 3/23/2018, 4/20/2018, 5/18/2019, and 6/22/2018 editions of Research Connections.
CTSI seeks applications for pilot, super-pilot projectsThe Pilot Studies Program of the Clinical and Translational Science Institute (CTSI) provides seed funding for highly innovative research that spans the translational spectrum. The Pilot Studies program is comprised of three categories of awards:
- Investigator-initiated pilot studies for faculty ($50,000 maximum for one year).
- Investigator-initiated pilot studies for trainees. Trainees are defined as graduate students, medical students, residents, postdocs, or fellows in University of Rochester training programs ($25,000 maximum for one year).
- UNYTE Translational Research Network grants ($50,000 maximum for one year).
View the Request for Applications (RFA).
The CTSI Incubator Program supports “super-pilot projects,” two years in duration, that are intended to accelerate innovative scientific discovery in the life sciences and public health, leading to new independently funded research programs. Each award is funded at a maximum level of $125,000 per year for each of two years.
View the Request for Applications (RFA).
Deadline for submission for both programs is August 27, 2018.
PhD dissertation defensesScott Kirila, mathematics, “Discrete Moments and Linear Combinations of L-functions.” 1 p.m. July 31, 2018. 1106A Hylan. Advisor: Steven Gonek.
Andrew Owens, chemistry, “Strategies for the Evolution of Macrocyclic Peptide Inhibitors of Protein-Protein Interactions.” 2 p.m. August 2, 2018. 1400 Wegmans Hall. Advisor: Rudi Fasan.
Zhuo Chen, physics and astronomy, “Evolution of low-mass symbiotic binaries.” 2:30 p.m., August 2, 2018. Bausch and Lomb 106. Advisor: Adam Frank.
Debra Saulnier, chemical engineering, “Liquid Crystal Chiroptical Polarization Rotators for the Near-UV Region.” 9 a.m. August 3, 2018. 4506 Wegmans Hall. Advisor: Mitchell Anthamatten.
Maureen Newman, biomedical engineering, “Bone-targeted Polymer Delivery of Osteoanabolics for Bone Regeneration.” 2 p.m. August 3, 2018. Medical Center 3-7619. Advisor: Danielle Benoit.
Mark your calendarJuly 30: The annual Kearns Research Symposium will take place in the Feldman Ballroom, Douglass Commons on the River Campus with oral presentations from McNair, BUILD, and IRIS scholars from 9 a.m. to 2 p.m., lightning talk presentations from all the NSF REU scholars, Xerox Fellows, and engineering McNair scholars from 2 p.m. to 4 p.m., and the research poster session from 4 p.m. to 5:30 p.m. All university community members are invited to attend and view the undergraduate research performed over the summer in our culminating research symposium event.
July 30: “Application of Natural Language Processing and Machine Learning to Capture Problems that Bother Patients,” lecture by Ira Shoulson, Grey Matter Technologies LLC. First in a new quarterly visiting lecturer series to foster sharing of new ideas in clinical research. Noon to 1 p.m., Ryan Case Method Room (1-9576). Presented by the Center for Health + Technology (CHeT) in conjunction with the Del Monte Institute for Neuroscience. Register here (no cost to attend) by Friday, July 27 if you plan on attending (lunch provided).
Aug. 1: Deadline to submit initial applications for Environmental Health Sciences Center funding of up to $30,000 for pilot projects relevant to the theme, “Environmental Agents as Modulators of Human Disease and Dysfunction.” Submit initial applications to Pat Noonan-Sullivan. Additional Information.
Aug. 13: Noon deadline to apply for Community Health Mini-Grants to be awarded in September by the Center for Community Health and Prevention. Up to $1,000 to address barriers to pursuing community health partnerships. Application directions for the grant can be found here. Contact Gail Hamilton via email or at 224-3062 for additional information.
Aug. 27: Deadline to apply to the Pilot Studies Program of the Clinical and Translational Science Institute (CTSI) for seed funding for highly innovative research that spans the translational spectrum in three categories: faculty, trainee, and UNYTE Translational Research Network. View the Request for Applications (RFA).
Aug. 27: Deadline to apply to the CTSI Incubator Program for “super-pilot projects,” two years in duration, that are intended to accelerate innovative scientific discovery in the life sciences and public health, leading to new independently funded research programs. Each award is funded at a maximum level of $125,000 per year for each of two years. View the Request for Applications (RFA).
Sept. 17: Deadline to apply for the Falling Walls competition. Winner of the Rochester competition, to be held October 2 in the Feldman Ballroom, will receive $500 and a trip to the Falling Walls Lab Finale in Berlin, November 7 to 9. Presenters will each have three minutes and three slides to summarize their groundbreaking ideas. Click here to register. Contact Adele Coelho, faculty outreach coordinator, at adele.coelho@rochester.edu for additional information.
Sept. 27: Workshop on Developmental Programming of Disease, focusing on current understanding of mechanisms that underlie early life programming. 8:30 a.m. to 5:30 p.m. Class of ’62 Auditorium. Offered by the Department of Environmental Medicine and the University’s Environmental Health Science Center. Free and open to all. Registration is requested for ordering refreshments. Read more here.
|
|
|
|
|