|
|
|
|
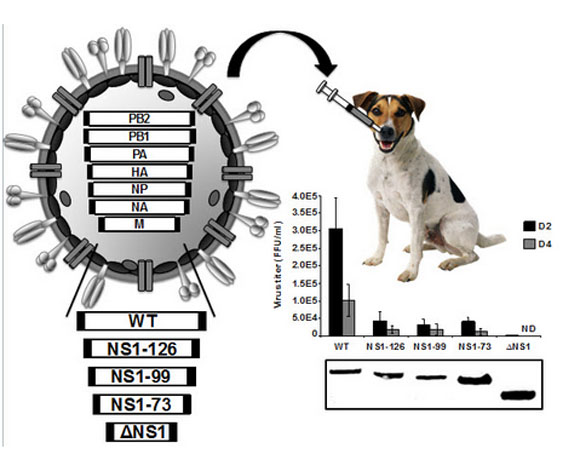 The lab of Luis Martinez-Sobrido used reverse genetics to alter canine influenza virus (shown at upper left) by truncating or deleting an NS1 protein, which significantly weakens the virus so that it elicits an immune response but doesn’t cause illness. Four altered forms of the virus – three encoding the first 73, 99, and 126 amino acids in NS1, and the other deleting NS1 altogether – along with the original wild type (WT) virus (all listed at lower left) were tested in mice and in canine tracheal tissue. The results at right show the markedly lower virulence of the NS1-truncated or deleted viruses, compared to wild type virus.
Canine influenza vaccine could protect people as wellUniversity researchers have developed, for the first time, two new vaccines for canine influenza – an accomplishment that is important for keeping humans safe as well. Dogs infected with multiple influenza viruses have the potential to act as “mixing vessels” and generate new flu strains that could infect people. Though this hasn’t happened yet, experts say it’s possible.
Today, veterinarians use canine vaccines that include inactivated or killed flu virus, but experts say they provide short-term, limited protection. Scientists led by Luis Martinez-Sobrido, associate professor of microbiology and immunology, created two “live-attenuated” vaccines against H3N8 canine influenza virus, which is currently circulating in dogs in the U.S. Past research shows that live-attenuated vaccines, made from live flu virus that is dampened down so that it doesn’t cause the flu, provide better immune responses and longer periods of protection.
Martinez-Sobrido’s team, including postdoctoral fellows Aitor Nogalez-Gonzalez and Laura Rodriguez, used a genetic engineering technique called reserve genetics to create a live vaccine that replicates in the nose, but not in the lungs. The nose is where the virus first enters a dog’s body, so generating an immune response there could stop the virus in its tracks. The study, published in the Journal of Virology, found the live vaccine was safe and able to induce better immune protection against H3N8 canine influenza virus in mice and dog tracheal cells than a commercially available inactivated vaccine.
In a second study highlighted in the journal Virology the team used reserve genetics to remove a protein called NS1 from H3N8 canine influenza virus. Previous studies have shown that deleting the NS1 viral protein significantly weakens flu viruses so that they elicit an immune response but don’t cause illness. This approach has been used with human, swine, and equine flu viruses to generate potential vaccines and was also safe and more effective than a traditional inactivated H3N8 influenza vaccine in mice and dog tracheal cells.
Both studies were performed in collaboration with Collin Parrish, professor of virology at the College of Veterinary Medicine at Cornell University and Pablo Murcia, professor at the University of Glasgow Center for Virus Research.
URMC-099 extends effectiveness of HIV therapiesA drug developed at the Medical Center extends the effectiveness of multiple HIV therapies by unleashing a cell’s own protective machinery on the virus. The finding, published in the Journal of Clinical Investigation, is an important step toward the creation of long-acting HIV drugs that could be administered once or twice per year, in contrast to current HIV treatments that must be taken daily.
The drug, called URMC-099, was developed in the laboratory of Harris A. (“Handy”) Gelbard, professor of neurology and director of the Center for Neural Development and Disease. When combined with “nanoformulated” versions of two commonly used anti-HIV drugs (also called antiretroviral drugs), URMC-099 lifts the brakes on a process called autophagy.
Normally, autophagy allows cells to get rid of intracellular “trash,” including invading viruses. In HIV infection, the virus prevents cells from turning on autophagy. This is one of the many tricks the virus uses to survive. When the brake on autophagy is lifted, cells are able to digest any virus that remains after treatment with antiretroviral therapy, leaving cells free of virus for extended periods of time.
“This study shows that URMC-099 has the potential to reduce the frequency of HIV therapy, which would eliminate the burden of daily treatment, greatly increase compliance, and help people better manage the disease,” said Gelbard, who has studied HIV/AIDS for the past 25 years. The finding builds on previous research that Gelbard conducted with Howard E. Gendelman, professor and chair of the Department of Pharmacology/Experimental Neuroscience at the University of Nebraska Medical Center.
Read more here.
Bridging Fellowships available through Humanities CenterFaculty members are now eligible to apply for Bridging Fellowships connected to the Humanities Center’s theme, which next year is “Memory and Forgetting.”
“The distinctive feature of Bridging Fellowships is that they are for study in an area that is peripheral to the fellow’s central professional concern, and they permit the acquisition of knowledge and methods in a different field,” the Faculty Handbook states.
Bridging Fellowships are ordinarily for one semester, and release fellows from teaching obligations during that period.
Joan Rubin, the Ani & Mark Gabrellian Director of the Humanities Center and Dexter Perkins Professor in History, says next year’s external and internal fellows (soon to be announced) will bring the perspectives of musicology, political theory, philosophy, literary and communication studies, and studio art to the center. In addition, visiting lecturers, with whom a Bridging Fellow might also seek to make connections, will likely include a historian, a neuroscientist, and a novelist.
“Faculty members who have a research project that could be enhanced by creative engagement with the approaches of those fields and with the center’s programs should talk to me right away if they wish to explore the possibility of a Bridging Fellowship to the Center,” says Rubin, who can be contacted at joan.rubin@rochester.edu. The deadline for proposals is mid-February.
Wilde is retired, but still mentoring others in her fieldThough Mary Wilde retired as a School of Nursing faculty member at the close of the 2016 academic year, she has barely slowed down. An international expert on improving the self-management of people using long-term catheters, Wilde is still collaborating with researchers around the world to sustain her comprehensive and ground-breaking work in the field.
For three decades, Wilde focused on identifying, understanding, and describing catheter-related problems from the perspective of the patient, and on developing effective self-management interventions. Catheter related-problems include urinary tract infection, blockage or obstruction of the catheter, accidental dislodgement, and leakage or bypassing of urine — all of which can cause considerable disruption for catheter users and their families’ daily routines, and contribute to excess health care expense.
Wilde, an emeritus professor, is continuing to disseminate the results of her studies, the last of which was a $421,000 R21 project that ended in April 2016, and remains a consultant with a team of researchers in the United Kingdom. She is also collaborating with a group of University nursing faculty members on a paper looking at the concept of self-monitoring in different clinical contexts.
Her research is so distinct that there are few if any scholars in the world who have tackled the subject as comprehensively as Wilde has. Most U.S. research has been oriented to address short-term catheter use in hospitals.
For her work to be sustained, it’s critical that she link to a new generation of researchers. To that end, she’s serving on the PhD committee of a nursing student at the University of Nebraska-Lincoln. She has also created online learning modules, which she shared at the International Continence Society meeting in Tokyo in September to promote dissemination and use of her research materials.
“Really, nobody’s working on self-management, nobody’s looking at catheter issues at the level and complexity that I have. I know that I can support researchers,” Wilde says.
Read more here.
Epstein writes on importance of mindfulnessAs a third-year Harvard medical student years ago, Ronald Epstein watched an experienced surgeon fail to notice that his 18-year-old patient’s kidney had turned blue. Epstein spoke up and the surgeon was able to repair the kidney as the operation was extended for an hour. In that same rotation, Epstein observed that a different surgeon was adept at shifting from autopilot to deliberate precision during an extremely complicated surgery. The difference between the two doctors left a lasting impression, he writes, and set the stage for his life’s work: to identify the qualities and habits that allow healthcare providers to be at their best.
In his new book, Attending: Medicine, Mindfulness, and Humanity, Epstein, a professor of family medicine, provides an inside look at how doctors think, illustrating his points with true stories. It is the first book for the general public about mindfulness in medical practice,
Epstein makes a case that being attentive, curious, and open-minded is a moral choice that also greatly improves the doctor-patient experience and impacts medical outcomes. Epstein believes that anyone—doctors and nurses, as well as patients and families—can learn to listen closely, set aside judgments, and take a more compassionate and conscientious approach to medical decisions and caregiving.
“I’m hoping that people see medicine through new eyes,” Epstein says of the book. “I also hope that people realize that mindfulness is not just for doctors, it’s for anyone. Setting aside expectations, the need to interpret or give advice and just listening and really understanding one another, is something that’s valuable for everyone.”
Epstein has built a worldwide reputation for physician training. He wrote a 2002 medical education article that is among the top-five most widely cited articles in the last century. It called for revamping the definition of “professional competence,” expanding it beyond knowledge of medicine and basic skills to include reasoning, judgment, time-management, communication skills, and the way doctors cope with ambiguity.
Read more here.
PhD dissertation defenseKhatera Rahmani, Toxicology, “CRM1 (Exportin 1) Inhibitors, Leptomycin B and Curcumin, Alter CRM1’s Subcellular Distribution.” 1 p.m., Feb. 13, 2017. Case Method Room (1-9576). Advisor: David A. Dean.
Mark your calendarFeb. 6: PONS Luncheon Roundtable Series: Alzheimer’s Disease and Dementia. Noon, Combined Northeastern Room 1-9525 & 1-9535 (URMC). Kerry O’Banion, (vice chair, Department of Neuroscience), Anton Porsteinsson, (William and Sheila Konar Endowed Professorship, Department of Psychiatry), and Robert Chapman, (professor, Department of Brain and Cognitive Sciences) will discuss the basic, systematic, and clinical AD research ongoing at UR. Refreshments will be provided. Hosted by the Pre-doctoral Organization for the Neurosciences (PONS). For more information on upcoming Neuro-related events, visit http://blogs.rochester.edu/pons/upcoming.
Feb. 8: “Introduction to Precision Health,” presented by Ying Meng, research associate at the School of Nursing. The promise of precision medicine is delivering the right treatments, at the right time, to the right person. Meng’s presentation will introduce the context of precision medicine illustrated by examples of pharmacogenetics. Nutrigenetics in the milieu of obesity will be further discussed. Noon to 1 p.m., Helen Wood Hall (1w304). School of Nursing Clinical and Research Grand Rounds.
Feb. 10: Noon deadline to apply for Center for Community Health mini-grants, which will be awarded in March 2017. Click here for the application form and instructions.
Feb. 27: 5 p.m. deadline to apply for Center for AIDS Research funding for projects that use the center’s Pharmacology Shared Resource to address key gaps in understanding HIV/AIDS pharmacology and therapeutics. Read more here.
March 20: Deadline to submit applications for a University Research Award of up to $37,500, matched by the applicant’s home school for a total of $75,000. The program provides seed money on a competitive basis for innovative research projects that are likely to obtain external support. Completed applications should be directed to adele.coelho@rochester.edu. Click here to view the full RFP.
March 20: Deadline to submit applications for an AS&E PumpPrimer II award. Click here for more information. Faculty in the School of Arts & Science should refer questions to Debra Haring, and those in the Hajim School of Engineering to Cindy Gary.
March 25: Brainstorming for the Healthy Weight Initiative, which aims to increase the proportion of people with healthy weight in Rochester and beyond. The goal is to identify potential collaborators and research topics in any area related to body weight development as a first step toward developing new transdisciplinary research teams to obtain more research funding. For more information, contact Diana Fernandez.
|
|
|
|
|