|
|
|
|
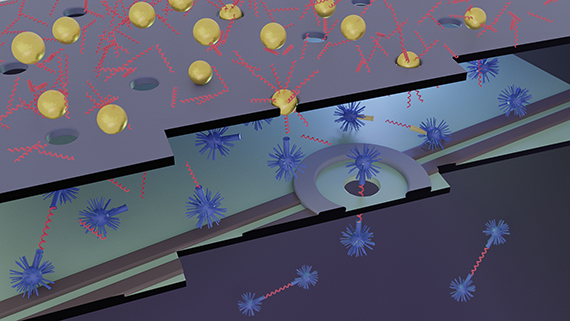 An inexpensive but highly sensitive biomarker detection system is being developed in a collaboration between the University of Rochester, the University of Ottawa, and Rochester-based SiMPore Inc. The team is using highly sensitive solid state nanopores to detect biomarkers of traumatic brain injury, bladder cancer, and other acute disorders in serum and urine. (University of Rochester illustration / Michael Osadciw)
Smaller is better for detecting biomarkers of trauma and cancerThe tiny proteins that can alert us to acute human disorders—traumatic brain injury (TBI), cancer, heart attack, and stroke—are freely circulating in our blood, urine, and other fluids. But these tiny “biomarkers” are also difficult and costly to detect.
James McGrath, professor of biomedical engineering, is helping to address this problem with Jonathan Flax, a Medical Center urologist; researchers at the University of Ottawa; and SiMPore, a University spin-out company that manufactures ultrathin membranes.
The collaborators have a received a $1.6 million grant from the National Institute of Biomedical Imaging and Bioengineering to develop a compact, portable, inexpensive biomarker detector using nanopore membranes and filters. The filters are so thin it would take more than 1,000 stacked on top of each other to equal the width of a human hair.
The device will be portable and nimble enough to produce results in a matter of minutes when used in the field by emergency responders, for example, to determine whether someone is suffering from traumatic brain injury.
Read more here about a collaboration that spans not only the River Campus and Medical Center, but two different universities, and academia and industry.
Mental illness and suicide among physiciansCOVID-19 is raising awareness of the fact that physicians are not immune to mental illness.
The pandemic has produced greater isolation. Hallway conversations that happened previously, group lunches, and all the socializing suddenly ended. That’s meant fewer ways for health care providers to process difficult experiences, leading to greater distress. The social support network that was once there suddenly vanished.
Ronald Epstein, professor in the Department of Family Medicine, along with other researchers are unpacking how mental illness affects health care professions and the barriers to getting treatment. Their article, titled Mental illness and suicide among physicians, recently appeared in The Lancet.
Across all countries, physicians have a much higher suicide rate than the general population and those of similar socio-economic status. The article points out that according to estimates in the United States, one doctor dies by suicide per day.
“Part of the culture of medicine is a culture of invincibility,” says Epstein. “Physicians are resilient but reluctant to ask for help. When we’re suffering, we do it alone and in silence. We need to make more public that physicians too suffer from anxiety, depression and post-traumatic stress.”
According to Epstein, the way forward consists of intervention at three important levels: the regulatory level, the institutional level, and the individual level. It’s key to ask, for example, what can institutions do to recognize and identify people who might be suffering? How can they change the working conditions so they’re less likely to make matters worse? Read more.
How to harness your stressReevaluating how one perceives stress can make a big difference to a person’s mental health, general well-being, and success, according to University of Rochester psychologists.
For their latest study, which appears in the Journal of Experimental Psychology: General, Rochester researchers trained adolescents and young adults at a community college to treat their stress response as a tool rather than an obstacle. The team found that in addition to reducing their anxiety, “good stress” mindset reset helped the students score higher on tests, procrastinate less, stay enrolled in classes, and respond to academic challenges in a healthier way.
To reframe their understanding of stress, the students completed a standardized reading and writing exercise that taught them that their stress responses had a function in performance contexts that applied directly to them, such as test taking.
“We use a type of ‘saying is believing’ approach whereby participants learn about the adaptive benefits of stress and they are prompted to write about how it can help them achieve,” says lead author Jeremy Jamieson, a Rochester associate professor of psychology and the principal investigator at the University’s Social Stress Lab. He researches how experiences of stress affect decisions, emotions, and performance. The study builds on his earlier research on optimizing stress responses. Read more.
Roc STAR pilot projects help aging patients, caregiversTwo researchers are recipients of 2021 Pilot Awards from the Medical Center’s Rochester Roybal Center for Social Ties & Aging Research (Roc STAR), co-sponsored with generous support from the UR Aging Institute.
Lee Kehoe, a postdoctoral fellow in the Clinical and Translational Cancer Control Research Training Program, received the ProtoSTAR Award for an early stage investigator to develop and test a dyadic life review intervention for individuals with advanced cancer and mild cognitive impairment and their care partners.
Benzi Kluger, the Julius, Helen, and Robert Fine Distinguished Professor in Neurology, has received the STAR Constellation Award to adapt and test a group program to promote social connection in caregivers of older adults with Dementia with Lewy Bodies (DLB). This novel program emphasizes peer support and positive psychology to encourage care partners to thrive in their role.
Ongoing pilot studies awarded in the 2020 Pilot Award Program are led by Caroline Silva, assistant professor in psychiatry, and Maria Quiñones, assistant professor in the School of Nursing, who are testing programs to increase social connection in Hispanic/Latino caregivers. Autumn Gallegos, assistant professor in psychiatry, is testing a smartphone-based mindfulness training program to promote social connection in caregivers.
Roc STAR is a research center focused on promoting the social well-being and healthy aging of those caring for a family member with Alzheimer’s disease or related dementia.
The next call for pilot proposals will be announced in the fall. To join the center’s listserv, email: rocstarcenter@urmc.rochester.edu.
Share your thoughts on strategic planning
Dias will give October 14 Huang Technology and Innovation presentationRanga Dias, assistant professor of mechanical engineering and physics and astronomy, will describe how his research has advanced the quest to achieve viable superconducting materials from noon to 1 p.m. October 14 during a virtual Huang Speaker Series in Technology and Innovation presentation.
The presentation, moderated by Gilbert ‘Rip’ Collins, associate director of science, technology, and academics at the Laboratory for Laser Energetics, will be an opportunity to find out about Dias’ ground-breaking research and just how close we might be to an energy-efficiency revolution, hover boards, and magnetically levitated trains.
The series is made possible by the generosity and vision of Robert Huang ’70 (MS), ’76M (MA). Learn more and register here.
Wilmot invites proposals for pilot research projectsThe Wilmot Cancer Institute invites proposals for pilot research projects that are responsive to Wilmot’s community outreach and engagement research priorities.
Responsive projects will investigate:
- risk or prognostic factors,
- prevention or risk reduction methods,
- biomarkers or disease outcomes,
- cancer control or survivorship interventions, or
- treatment approaches relevant to these priorities.
Investigators are encouraged to take advantage of existing tissue samples and data derived from catchment area populations. Read more about Wilmot’s Community Outreach and Engagement Program.
Applicants must be members of Wilmot Cancer Institute. Project concept summaries are due Friday, Oct. 29 and a “shark-tank” style review process will take place on Tuesday, Nov. 16.
Applicants are strongly urged to attend an Oct. 11 pre-meeting to discuss catchment area research priorities and the shark tank process or view the recorded video of the session available in Box.
Projects may start as early as Dec. 1, 2021 and end no later than June 30, 2022.
Download the RFA for additional details, including a list of COE priorities. Contact Thomas_Fogg@urmc.rochester.edu with questions on the application process, or Charles_Kamen@urmc.rochester.edu with questions about COE priorities.
Next generation sequencing mini-course offeredHosted by the Medical Center’s Genomics Resource Center in collaboration with Illumina, this four-part course, starting Oct. 19, provides a foundation in the principles of next-generation sequencing and serves as a pre-requisite for advanced seminars in the spring. Learn more and register here.
|
|
|
|
|