Rochester scientists are restoring the brain’s trash disposal system with a drug currently used to induce labor.
Alzheimer’s, Parkinson’s, and other neurological disorders can be seen as “dirty brain” diseases, where the brain struggles to clear out harmful waste. Aging is a key risk factor because, as we grow older, our brain’s ability to remove toxic buildup slows down. However, new research in mice demonstrates that it’s possible to reverse age-related effects and restore the brain’s waste-clearing process.
“This research shows that restoring cervical lymph vessel function can substantially rescue the slower removal of waste from the brain associated with age,” says Douglas Kelley, a professor of mechanical engineering at the University of Rochester. “Moreover, this was accomplished with a drug already being used clinically, offering a potential treatment strategy.”
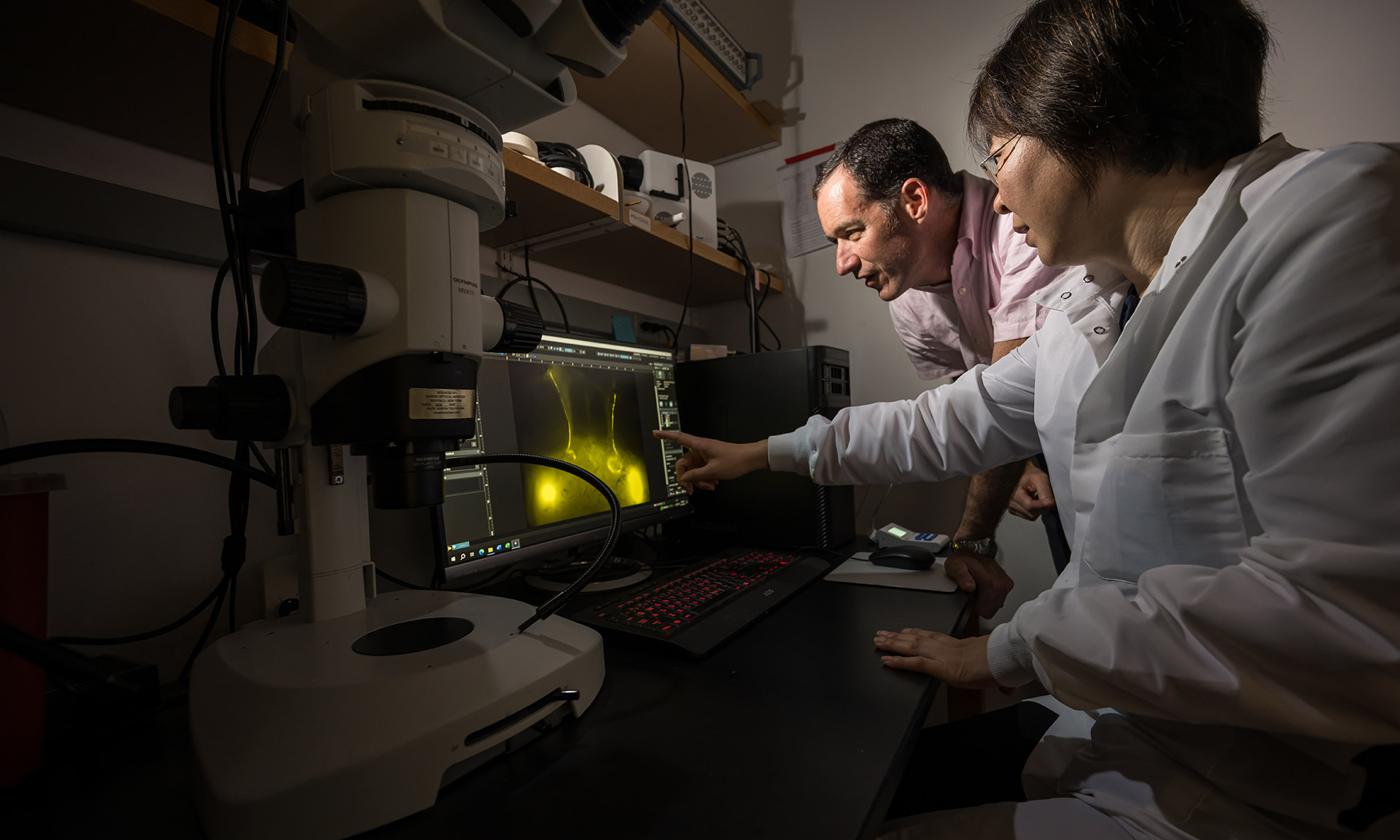
Kelley is one of the lead authors of the study, which appears in the journal Nature Aging, along with Maiken Nedergaard, codirector the University’s Center for Translational Neuromedicine. The study is one of many collaborations carried out by researchers at Rochester’s Hajim School of Engineering & Applied Sciences and the Medical Center.
First described by Nedergaard and her colleagues in 2012, the glymphatic system is the brain’s unique waste removal process that uses cerebrospinal fluid (CSF) to wash away excess proteins generated by energy-hungry neurons and other cells in the brain during normal activity. The discovery pointed the way to potential new approaches to treat diseases commonly associated with the accumulation of protein waste in the brain, such as Alzheimer’s (beta amyloid and tau) and Parkinson’s (alpha-synuclein). In healthy and young brains, the glymphatic system does a good job of flushing away these toxic proteins; however, as we age, this system slows, setting the stage for these diseases.
A network of tiny pumps draws waste from the brain
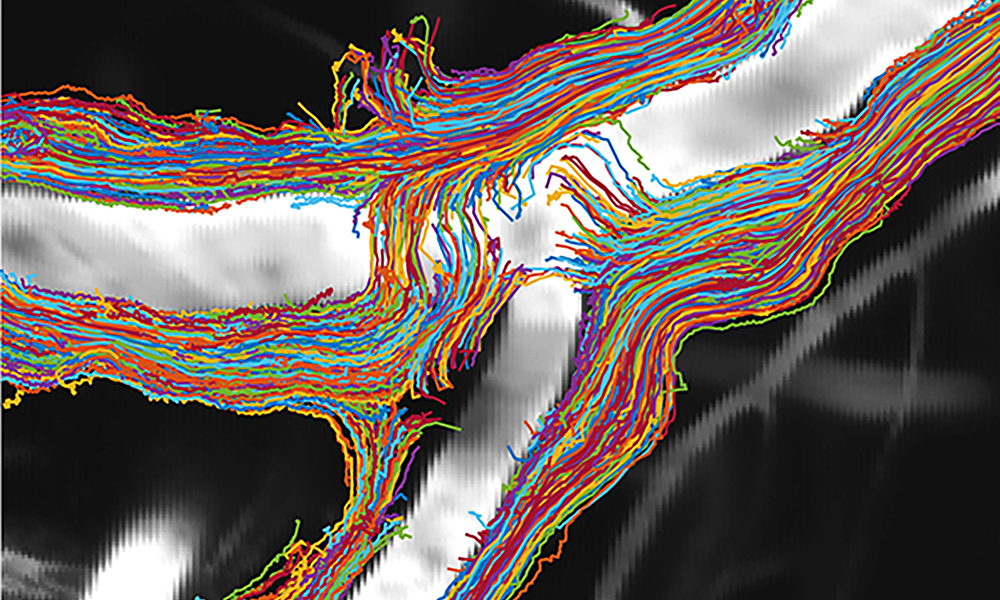
Once laden with protein waste, CSF in the skull needs to make its way to the lymphatic system and, ultimately, to the kidneys, where it is processed along with the body’s other waste. The new research combines advanced imaging and particle-tracking techniques to describe for the first time in detail the route by way of the cervical lymph vessels in the neck through which half of dirty CSF exits the brain.
In addition to measuring the flow of CSF, the researcher team—including study first authors Ting Du, Aditya Raghunandan, and Humberto Mestre—were able observe and record the pulsing of lymph vessels in the neck that helps draw CSF out of the brain. “Unlike the cardiovascular system, which has one big pump—the heart—fluid in the lymphatic system is instead transported by a network of tiny pumps,” says Kelley. These microscopic pumps, called lymphangions, have valves to prevent backflow and are strung together, one after another, to form lymph vessels.
The researchers found that as the mice aged, the frequency of contractions decreased, and the valves failed. As a result, the speed of dirty CSF flowing out of the brains of older mice was 63 percent slower compared to younger animals.
Known drug restarts flow of brain-cleaning fluids
The team then set out to see if they could revive the lymphangions and identified a drug called prostaglandin F2α, a hormone-like compound commonly used medically to induce labor and known to aid smooth muscle contraction. The lymphangions are lined with smooth muscle cells, and when the researchers applied the drug to the cervical lymph vessels in older mice, the frequency of contractions and the flow of dirty CSF from the brain both increased, returning to a level of efficiency found in younger mice.
“These vessels are conveniently located near the surface of the skin. We know they are important, and we now know how to accelerate function,” says Kelley. “One can see how this approach, perhaps combined with other interventions, could be the basis for future therapies for these diseases.”