Rochester undergraduates have developed a fast, noninvasive, affordable, and eco-friendly way to diagnose sepsis, a life-threatening medical complication.
Sepsis definition and facts
What is sepsis?
Sepsis is an extreme response to an infection; when the body’s immune response to an infection starts doing more damage to the body than to the infection, the body is in sepsis. Sepsis can cause shock and life-threatening organ dysfunction.
What causes sepsis?
Bacterial infections—such as urinary tract or skin infections or infections in the intestines—cause most cases of sepsis, although sepsis can also be a result of viral infections.
What are the symptoms of sepsis?
Although the symptoms of sepsis may look like other health conditions, the main symptoms include fever or chills, rapid breathing, vomiting, fast heart rate, and confusion or disorientation.
- Get more information about sepsis from UR Medicine.
Every year, approximately 1.7 million American adults develop sepsis, a life-threatening complication that arises when the body has an overwhelming immune response to an infection. According to the Centers for Disease Control and Prevention, sepsis causes more than 20 percent of all deaths worldwide and one in every three deaths in US hospitals.
A crucial aspect of treating sepsis is to catch it at an early stage when a patient’s infection is still curable. Current methods to diagnose sepsis, however, rely on tests that can take days to yield results, while early sepsis can turn into full-blown septic shock within only one hour after the first symptoms emerge.
In order to address this problem, a team of 12 undergraduate students at the University of Rochester developed a novel device that instantaneously diagnoses sepsis based on biomarkers in a person’s sweat. The device offers a noninvasive way to monitor sepsis in real-time and uses materials that are environmentally friendly and affordable, making the device easily deployable in low-income countries.
The team recently entered their device in the International Genetically Engineered Machine (iGEM) competition, where it was nominated for best diagnostics project, best hardware, and best education awards and won a gold medal, making the team the second-most-awarded iGEM team in North America.
“After researching statistics on sepsis and talking to a variety of medical experts, we got a sense of its immense medical and economic impacts and the need to develop better options for sepsis diagnosis,” says iGEM team member Amanda Adams ’22, a biomedical engineering major. “Our goal was to create a biosensor that could provide up-to-date information about a patient’s condition. Getting to work in a student-led team where we were directly responsible for the entire project from planning it to presenting it was very rewarding.”
Worldwide synthetic biology competition
In 2020, Rochester launched an undergraduate class composed of students who compete in a worldwide synthetic biology competition with the goal to solve a real-world problem using innovative biological ideas. (Synthetic biology involves creating new biological parts or systems using materials already found in nature.) During the iGEM competition, held in mid-November, the undergraduates present to a panel of judges the projects they have spent the year designing and implementing.
“This year’s iGEM team tackled a problem that has a huge impact on society,” says Anne S. Meyer, an associate professor of biology, and one of the advisors for Rochester’s iGEM team. “The students realized that a patient’s sweat contains specific biomarkers that can report on whether or not the patient has sepsis. So, monitoring the levels of these biomarkers in patient sweat would be an easy and noninvasive way to diagnose sepsis in real time to get instant information.”
Overcoming the limitations of current sepsis diagnostic tools
Doctors use many different tools to diagnose patients, one of which is the presence and concentration of certain biomarkers—molecules such as proteins or sugar that are associated with a particular disease, condition, or biological process. There are several ways to measure biomarker concentrations, including test strips and lab-on-a-chip devices, but many of these approaches only show biomarker concentrations at one specific point in time. These methods can also be expensive, and many take hours to perform.
“This means that doctors often need to wait for the results of a test, and the results may not even be accurate if the patient developed a condition after the sample was taken,” Adams says.
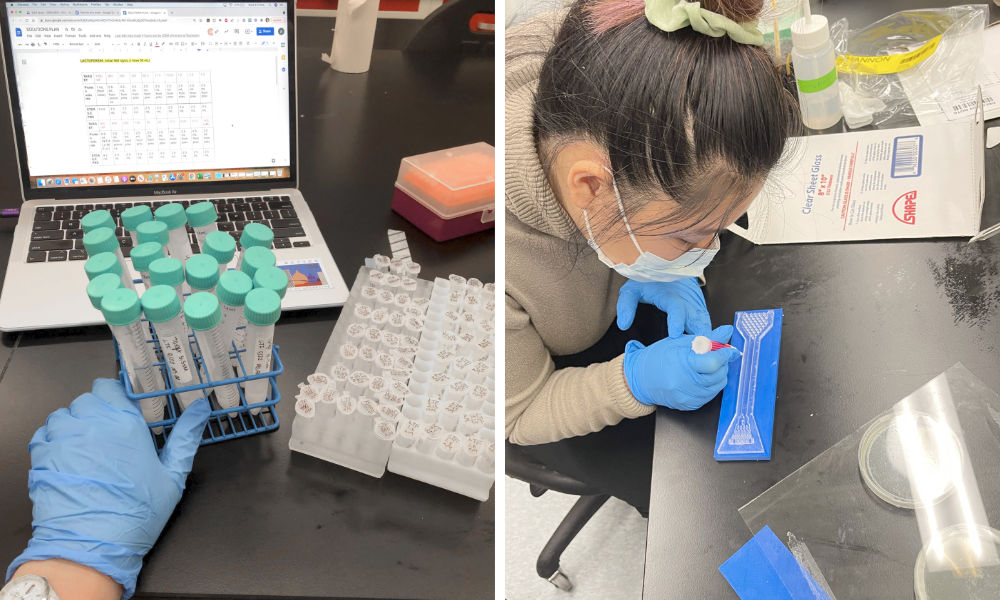
The Rochester students consulted with sepsis survivors, scientists, and clinicians at the University of Rochester Medical Center to design a sepsis-sensing device, which they named “Bio-Spire,” a combination of “biology” and “perspire.” Bio-Spire is a biosensor that continuously monitors the levels of biomarkers in sweat. Unlike blood, sweat is a noninvasive medium to collect, and unlike saliva or urine, biomarkers in sweat can be continuously analyzed. The levels of biomarkers in blood and in sweat are correlated, so changes in the amount of biomarkers in sweat are indicative of changes in the blood.
That is, a change in biomarker levels in a patient’s sweat can signify a deterioration of the patient’s condition—and may signify sepsis.
Designing a ‘game-changer’ diagnostic device
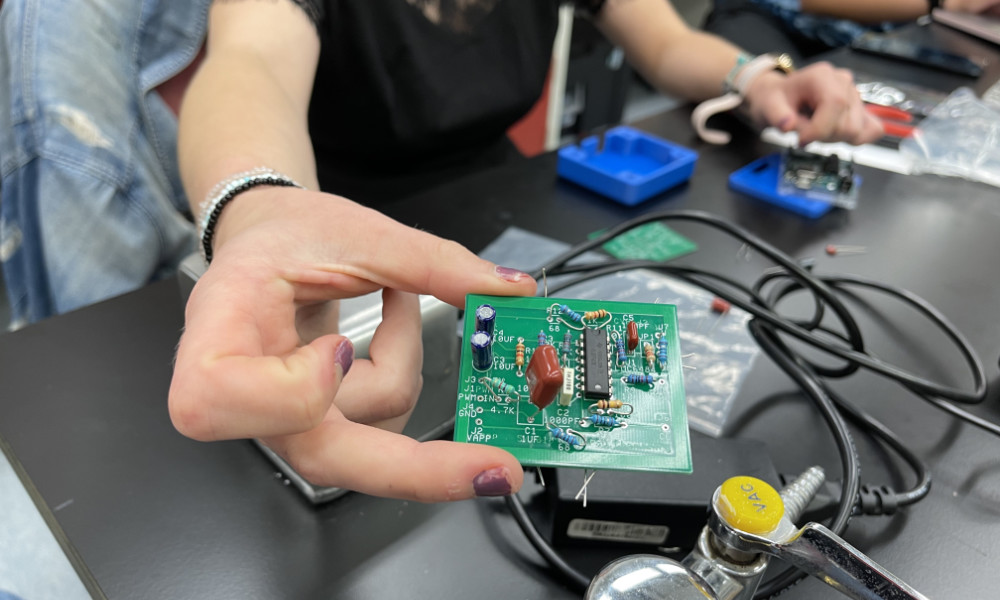
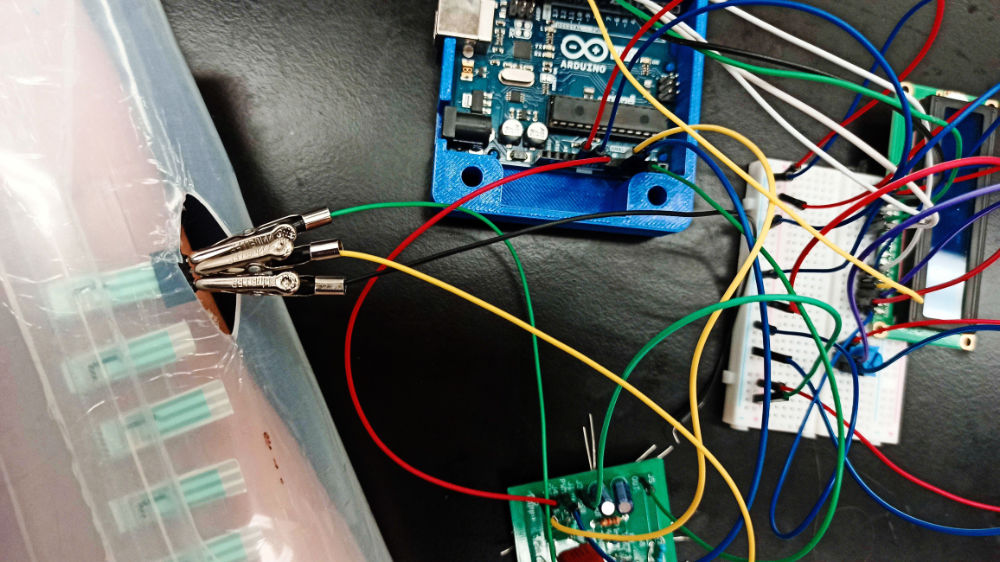
Bio-Spire is designed to collect a tiny amount of sweat from a patient’s skin and wick the sweat past an integrated set of electrodes covered in biomarker detectors. The biomarker detectors consist of short pieces of DNA receptors attached to a small sheet of graphene—an ultra-thin layer of material that is highly conductive. The students synthetically created their own graphene and DNA in an environmentally-friendly manner by using engineered biological components.
When the sleeve-like device is placed on a patient’s arm, biomarkers associated with sepsis bind to the DNA receptors, changing the conductivity of the graphene sheet and triggering an electrical resistance in the electrodes, which is then recorded on a computer. The students created software that displays the concentrations of sepsis biomarkers in real time, permitting health care workers to receive up-to-the-minute updates on a patient’s condition.
“The Rochester team’s real-time sepsis diagnosis device is a game-changer because all of its parts can be created in an accessible, inexpensive way,” Meyer says. “Plus, it is the fastest sepsis diagnostic device ever created.”
In addition to developing the device, the team worked to increase awareness of sepsis and synthetic biology in the local community and beyond through a variety of education and outreach programs, including interactive science lessons with children’s summer camps in Rochester. The team also collaborated with an iGEM team from the Ohio State University to virtually publish a children’s book called A Trip to the Hospital: Randall’s Lesson on Sepsis, which is available on Amazon and Apple Books.
“We are excited by the promising results of this project and honored to be recognized for our efforts in addressing such an important, interdisciplinary issue in the medical community,” Adams says.
Because iGEM is an open-source competition, the team’s work is documented and available on their Bio-Spire Wiki page. This format allows future students or developers to take up the design and build upon the ideas.