In Review
 MIND AND BODY: Psychological factors play a role in physical frailty, according to a new Rochester study. (Photo: Adobe Stock)
MIND AND BODY: Psychological factors play a role in physical frailty, according to a new Rochester study. (Photo: Adobe Stock)Biologists, geneticists, and other scientists who study the cellular processes of aging have long focused on a gene known as sirtuin 6 (SIRT6)—so much so that it’s been identified as a “longevity gene.”
SIRT6 helps repair DNA that’s been damaged as a result of normal chemical processes in cells. But so far, investigators have been unable to determine what triggers the gene.
Rochester biologists Vera Gorbunova and Andrei Seluanov say they’ve discovered a clue: a protein that appears to play a role in activating SIRT6, setting in motion a cascade of molecular activity to repair damaged DNA.
To find out what activates SIRT6, the researchers alternately applied chemical inhibitors to human skin cells to determine which proteins were essential in getting the gene to repair broken DNA strands. They discovered that one protein was involved in activating the gene in response to oxidative stress—c-Jun N-terminal kinase, or JNK. When JNK was inhibited, SIRT6 was not activated, and the broken strands of DNA were not repaired efficiently.
The study, published in the journal Cell Reports, is the latest by Gorbunova and Seluanov to shed light on the molecular mechanisms that drive the aging process. While more research and clinical work need to be done, such studies might allow pharmaceutical researchers to one day design drugs that activate SIRT6 in ways that reduce molecular damage.
“These drugs may be used to protect our genomes from damage, and could ultimately prevent cancer and extend healthy lifespan,” says Seluanov.
—Peter Iglinski
Helping the Frail Elderly Means Looking Beyond Physical Ailments
A new study published in the Journals of Gerontology suggests that the physical frailty experienced by about one in 10 people over age 65 is influenced by psychosocial factors, including chronic stress, socioeconomic status, and how much control they believe they have over their own lives.
Christopher Mooney ’10M (MPH), ’16W (PhD) and collaborators from the Warner School of Education and the Medical Center found that chronic stress is associated with feeling less control—and that, in turn, is associated with greater physical frailty. Similar results were found for the effects of poverty, and the findings were the same across age, gender and racial subgroups.
The results, says Mooney, have important implications for interventions aimed at making people less frail and improving the health of those at risk of frailty. The study is one of the first to investigate the effects of chronic stressors on physical frailty.
—Theresa Danylak
Treatment Possible for Rare Form of Muscular Dystrophy
The findings of a new Rochester study could pave the way for the first U.S.–approved treatment for Duchenne muscular dystrophy.
A condition found almost exclusively in boys, Duchenne muscular dystrophy is characterized by muscle weakness that rapidly leads to significant disability and ultimately affects other areas, including the heart and muscles responsible for breathing. An estimated 28,000 people in the United States are affected by the disease, which is often fatal by the time a patient reaches the late teens.
“Duchenne muscular dystrophy patients have limited treatment options and a desperate need for effective therapies,” says Medical Center neurologist Robert Griggs. He’s the lead author of a study showing that a corticosteroid known as deflazacort is a safe and effective treatment to combat the disease’s progression. The study is published in the journal Neurology.
Approved for use in Europe and elsewhere, deflazacort has never been through the approval process of the U.S. Food and Drug Administration (FDA). Although the drug was the subject of a clinical trial in the United States in the mid-1990s, soon after the trial was completed, the company sponsoring the research lost interest and the study results were never published.
At the urging of patients and families, Griggs—a professor of neurology, medicine, pathology and laboratory medicine, and pediatrics—and others have spent years trying to get access to the original study. The new data is their effort to recreate it.
Two new drug applications based on the study are now before the FDA.
—Mark Michaud
 PAINFUL: A popular nasal spray has been shown to be ineffective against the flu. Rochester scientists are helping fill the
treatment void. (Photo: AP Images)
PAINFUL: A popular nasal spray has been shown to be ineffective against the flu. Rochester scientists are helping fill the
treatment void. (Photo: AP Images)Progress toward a New Flu Vaccine
A rare mutation in a protein encoded by an influenza virus may be useful in developing a new live vaccine, according to Medical Center researchers.
The mutation weakens the flu virus by rendering the flu-encoded protein, called Non-Structural 1, or NS-1, defunct. The flu virus needs the encoded protein to prevent the immune system from alerting the host cell that it has been infected. Inhibiting the immune system affords the virus time to multiply and spread before the system can mount an attack.
Most people have healthy immune responses and would quickly and easily fend off a weakened mutant strain of flu. But a tiny percentage of people have an immune system defect that allows the mutant virus to replicate.
David Topham, the Marie Curran Wilson and Joseph Chamberlain Wilson Professor of Microbiology and Immunology, and Marta Lopez de Diego, research assistant professor of microbiology and immunology, say the NS-1 mutation has been found in just 0.03 percent of all flu strains reported in a national database. The pair isolated the mutated virus from a nasal swab of a single flu sufferer who happened to be among the small percentage of people with inadequate immune responses.
Now that they have isolated the virus, Topham and Diego hope that the naturally occurring attenuated virus can be used to create a new live flu vaccine. A new live vaccine would be particularly advantageous, as the Centers for Disease Control and Prevention stopped recommending use of the live attenuate flu vaccine FluMist earlier this year. Several studies found that the pain-free nasal spray, which was used in about one-third of young children in the U.S., offered no protection to that especially vulnerable population.
The study, published online in the Journal of Virology, also highlights the importance of flu virus surveillance—research in how the flu is changing, what flu mutations are circulating in humans and animals, and how those mutations affect virus function. Until recently, researchers believed that proteins like NS1 did not change much from strain to strain, or from season to season. But Topham’s study and others like it show that NS1 mutations occur naturally, and can affect the protein’s ability to suppress immunity. Monitoring for such mutations in nature could lead to more effective vaccines.
—Susanne Pallo
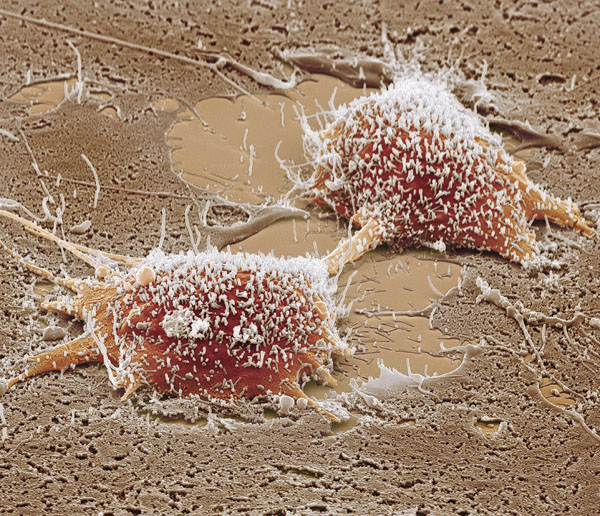 GLUTAMINE GLUTTONS: Cancer cells devour glutamine in order to replicate. They do it by fermenting sugar, according to a new
study. (Photo: Science Source)
GLUTAMINE GLUTTONS: Cancer cells devour glutamine in order to replicate. They do it by fermenting sugar, according to a new
study. (Photo: Science Source)Looking at Cell Metabolism, Finding Clues to Cancer
Cancer cells have their own unique ways of reproducing, involving a shrewd metabolic reprogramming that has been observed in virtually all types of cancer, but not in normal cells. In an article published in Cell Reports, Medical Center scientists show for the first time how cancer-causing mutations control and alter the way cancer cells biosynthesize and replicate.
The discovery is the result of a collaboration between the laboratories of Joshua Munger, associate professor of biochemistry and biophysics, and Hucky Land, the Robert and Dorothy Markin Professor and chair of biomedical genetics and director of research at the Wilmot Cancer Institute.
“Every tissue or cell type in the body has different metabolic needs. But as cells become cancerous their metabolism shifts in ways that are very different from normal cells,” Munger says. Identifying those differences is critical to developing treatments.
It’s been known for decades that cancer cells siphon glucose from the bloodstream at alarming rates. But cancer’s sugar addiction is only one part of the story. While sugar is the primary source of fuel for biosynthesis of normal cells, cancer cells switch from burning to fermenting sugar—a process that Land and Munger say is driven by cancer-causing mutations.
They also discovered that sugar fermentation in cancer cells facilitates their consumption of glutamine. Glutamine is abundantly available in the bloodstream, and cancer cells take in large amounts of it to support cell division.
“Our paper demonstrates that cancer cells, but not normal cells, depend on this link between sugar fermentation and glutamine consumption,” Land says. “This suggests a novel way that we might be able to intervene with treatment.
Bradley Smith, a scientific staff member in the Land lab, led the experiments, which were conducted with colon cancer cells. Preclinical data show that by blocking enzymes that are specific to colon cancer cell metabolism, tumor growth is slowed or stopped.
“Is it possible to apply this to other cancers? That’s our next question,” Munger says. “We’re testing how this could be broadly applied in the clinic.” —Leslie Orr

